First Trimester Meal Plan That Actually Works: What I Learned After My Perfect Nutrition Plans Fell Apart

When I first got pregnant, I thought I had this whole nutrition thing figured out. I was that person meal-prepping on Sundays, taking my vitamins religiously, feeling pretty smug about my healthy habits. Then week 6 hit, and suddenly the sight of my carefully planned kale salad made me want to cry. Everything I thought I knew about eating well? Yeah, that went straight out the window along with my ability to stomach anything green.
Most people don’t need extra food during pregnancy until the third trimester, when they should get around 200 more calories a day according to Tommy’s. This reality challenges the common myth of “eating for two” and highlights why understanding what your body actually needs matters more than just eating more food during your first trimester.
I’ll be honest – I tried to force myself to eat spinach smoothies for three weeks straight because I read they were “optimal.” All I got was green-tinted morning sickness and a serious aversion to my blender. It wasn’t until I started paying attention to what my body was actually telling me – and learning some surprising things about how pregnancy changes everything – that things started to click.
For expectant mothers wondering about safe caffeine limits during pregnancy, understanding how your changing body processes nutrients becomes even more important, since caffeine affects how well you absorb essential vitamins and minerals.
Table of Contents
- Why Everything I Thought I Knew About Eating Was Wrong
- Working With Your Body’s New Rules Instead of Against Them
- The Baby Development Stuff That Actually Matters (Without the Panic)
- Managing Inflammation Without Going Crazy
- Eating for Two Without Actually Eating for Two
- The Nutrient Combinations That Made a Real Difference
- Final Thoughts
TL;DR
- Your body has natural energy dips every 2-3 hours – work with them instead of fighting them with caffeine
- That morning energy surge? Perfect time for protein, not just toast
- Your gut bacteria can actually make some nutrients your baby needs – if you feed them right
- Meal timing affects your baby’s development, but you’re not responsible for programming their entire future
- The ratio of different fats matters more than just eating “healthy fats”
- Not eating between dinner and breakfast (aka normal sleeping) can actually help your baby’s brain development
- Some nutrient combinations work way better together than alone
Why Everything I Thought I Knew About Eating Was Wrong
When I got pregnant, my body basically threw out the rulebook. One day I could eat anything, the next day the smell of my favorite coffee made me want to hide under the covers. Turns out, there’s actually science behind this chaos.

All those pregnancy hormones aren’t just making you tired and nauseous – they’re actually changing how your body processes food. It’s like your digestive system got a software update overnight, except nobody gave you the manual.
You could be eating all the “right” foods and taking the best prenatal vitamins, but if your timing is off with your body’s new rhythm, you might be missing out on actually feeling good. During the first trimester, when your baby’s brain and spine are forming, every bit of optimization helps – but it doesn’t have to be perfect.
Here’s what I wish someone had told me: you don’t need to become a nutrition scientist. You just need to start paying attention to patterns and work with your body instead of against it.
Working With Your Body’s New Rules Instead of Against Them
Those Energy Crashes Are Actually Your Friend
Here’s what I wish someone had told me: your body has natural energy dips every few hours during pregnancy. Instead of fighting these with caffeine (which made my nausea worse), I started working with them. When I felt that familiar afternoon crash, I’d have some nuts with an apple. Simple, but it made a huge difference.
Those energy dips you’re experiencing every few hours? They’re actually your body’s way of saying “hey, now would be a good time for some healthy fats.” While pregnancy hormones slow down your digestion (hello, pregnancy constipation), they also create windows where your body is primed to absorb vitamins A, D, E, and K.
Look, I’m not saying you need to become a data scientist about your snacks. But maybe just notice – do you crash around 2 PM? Do you feel weird and shaky before lunch? Once you start paying attention, you can work with your body instead of against it. Some days I’d have my avocado toast at exactly the right time, other days I’d forget and eat cereal at 10 PM. Both are fine.
What actually worked for me:
- Notice when you naturally get tired (usually every 2-3 hours)
- Have something with healthy fats during these times
- Take your prenatal vitamins with these meals – they absorb better
Sarah, a friend who was pregnant around the same time, noticed she crashed every afternoon around 2 PM and again around 5 PM. Instead of reaching for coffee, she started eating a small handful of mixed nuts with an apple at 2 PM and having her dinner salad with olive oil dressing at 5 PM. Within a week, she told me she felt way more steady energy-wise.
Morning Protein: The Game-Changer I Didn’t See Coming
That morning energy surge you sometimes get? It’s actually the perfect time for protein, not just toast. Between 7-9 AM, your body is primed to take amino acids and turn them into building blocks for your rapidly developing baby.
I used to grab a piece of toast and call it breakfast. Now? I try to get some complete protein within 30 minutes of waking up. Scrambled eggs with spinach, Greek yogurt with hemp seeds, or even a protein smoothie with leafy greens. The sustained energy and reduced nausea were game-changers.
My morning routine (when I could manage it):
- Some kind of complete protein within 30 minutes of waking
- Pair it with B-vitamin rich foods (leafy greens, eggs work double duty here)
- Skip the simple carbs during this time to avoid energy crashes later
What surprised me most was how much this helped with morning sickness. Stable blood sugar from quality protein seemed to calm my queasy stomach better than crackers ever did. Though let’s be real – some days crackers in bed were all I could manage, and that’s okay too.
Your Gut Bacteria Are Working Overtime (And You Can Help)
Feeding the Good Guys
Your gut bacteria are working overtime during pregnancy, and they can actually manufacture some nutrients your baby needs – if you feed them right. Jerusalem artichokes and chicory root became my evening go-tos because they feed the specific bacteria that produce folate and vitamin K.
The timing thing was something I stumbled onto by accident. I’d have these prebiotic foods with dinner, then follow up with fermented foods like kefir or sauerkraut the next morning. It created this nice cycle where the good bacteria could grow overnight and then get reinforced.
While focusing on gut health, it’s also worth exploring simple ways to improve digestion during pregnancy, since digestive comfort directly impacts how well you absorb nutrients.
What worked for me:
- Jerusalem artichokes or chicory root with dinner (when I could find them)
- Follow with probiotic-rich foods the next morning
- Switch to gentler options when my system couldn’t handle the stronger stuff
Some days my system couldn’t handle the stronger prebiotics, so I’d switch to gentler options. Cooked and cooled potatoes or green bananas worked well. The key was consistency, not perfection.
Rethinking Morning Sickness
Morning sickness isn’t just about hormones – it’s often linked to what’s happening in your gut. Instead of just avoiding trigger foods, you can actually work to rebalance things.
Ginger alone never helped my nausea much, but ginger combined with prebiotic fibers? That was different. Small amounts of fermented foods throughout the day, rather than large servings, seemed to gradually shift things in the right direction.
My nausea-fighting strategy:
- Combine ginger with prebiotic fibers (not alone)
- Use fermented foods in small, frequent doses
- Avoid antimicrobial foods during the worst nausea periods
The improvement wasn’t immediate, but after about two weeks of consistent gut support, my morning sickness became much more manageable. Not gone, but manageable.
Recent research from nutritionist Ramya B at Cloudnine Group of Hospitals emphasizes that “The early pregnancy period is when organ development begins and continues to grow. This period is crucial because certain nutrients play a major role in organ development”, highlighting why supporting your gut health matters even more when morning sickness makes eating challenging.
The Baby Development Stuff That Actually Matters (Without the Panic)
I know this might sound intense, but here’s the thing – you’re not responsible for programming your kid’s entire future health with every bite you take. What you CAN do is give them a good foundation. Think of it like this: you’re not building the whole house, you’re just laying some solid groundwork.
The first trimester isn’t just about growing a baby – it’s about setting up patterns that will influence how your baby’s genes are expressed. But before you start panicking about every meal choice, remember that your baby is incredibly resilient.

Working With Your Natural Rhythms
The Morning Blood Sugar Thing
Your blood sugar naturally spikes when you wake up (it’s called the dawn phenomenon), and pregnancy makes this even more pronounced. Instead of fighting it, I learned to work with it by having 20-25g of complete protein within an hour of waking.
This gives your baby’s developing brain the amino acids it needs during this natural glucose surge. The combination creates good conditions for neural development.
My dawn routine (when I could manage it):
- 20-25g complete protein within 1 hour of waking
- Pair with complex carbs to stabilize things
- Monitor how you feel and adjust accordingly
I started tracking my patterns and noticed that when I nailed this morning routine, I had more stable energy throughout the day and fewer afternoon crashes.
| Time | Protein Source | Amount | What I Paired It With |
|---|---|---|---|
| 7:00 AM | Greek yogurt | 3/4 cup (20g protein) | 1/2 cup berries |
| 7:30 AM | Scrambled eggs | 3 eggs (21g protein) | 1 slice whole grain toast |
| 8:00 AM | Protein smoothie | 1 scoop protein powder (25g) | 1 banana + oats |
| 8:30 AM | Cottage cheese | 3/4 cup (22g protein) | 1/4 cup granola |
Setting Up Your Baby’s Sleep Patterns Before They’re Born
The melatonin you produce crosses the placenta and helps establish your baby’s sleep-wake cycles before they’re even born. Your evening meal becomes a tool for potentially helping your future baby’s sleep patterns.
Tryptophan-rich foods became my evening staples. Turkey and pumpkin seeds, combined with complex carbs to help tryptophan cross into the brain. But timing matters – you need to eat these 3-4 hours before bed for optimal melatonin production.
My evening routine:
- Include tryptophan-rich foods 3-4 hours before bed
- Pair with complex carbs for better uptake
- Try to avoid screens during evening meals (easier said than done)
The bonus? Better sleep for me meant better development conditions for baby. Win-win.
Beyond Basic Folate
According to the American College of Obstetricians and Gynecologists, the requirement of folic acid during pregnancy is 600µg/day, but getting the most out of your folate requires more than just taking a supplement.
The Choline and Folate Team-Up
Everyone talks about folate for neural tube development, but choline is equally important – and they work together in ways that most advice completely misses. I started combining egg yolks (loaded with choline) with leafy greens (folate powerhouses) in single meals.
These nutrients support each other’s absorption and work together in reactions that are crucial for your baby’s DNA development.
My go-to combinations:
- Egg yolks with leafy greens in single meals
- Add sunflower lecithin to smoothies with spinach
- Time these combinations with your prenatal vitamin
My favorite became a spinach and mushroom omelet or a green smoothie with sunflower lecithin. Simple combinations that actually made a difference.
Maria, another mom I know, discovered that her folate levels stayed low despite taking supplements until she started making a daily green smoothie with spinach, one whole egg, sunflower lecithin, and banana. Within six weeks, her bloo d work showed significant improvement, and she felt more energetic throughout her first trimester.
Managing Inflammation Without Going Crazy
I used to think I needed to eliminate all inflammation, like I was some kind of anti-inflammatory warrior. Spoiler alert: that’s impossible and probably not even good for you. Turns out, your body needs some inflammation during pregnancy – it’s part of the process. The goal isn’t perfection, it’s balance.
Inflammation during pregnancy is tricky. You need some for proper implantation and placental development, but too much can interfere with fetal growth. Finding that sweet spot became about supporting healthy responses without going overboard.
The Fat Balance That Actually Matters
Timing Your Anti-Inflammatory Foods
Your inflammatory response follows predictable patterns during early pregnancy. I discovered that having omega-3 rich foods in the evening seemed to work better than morning intake, possibly because inflammation naturally peaks at certain times.
Avoiding processed omega-6 oils during morning hours, when cortisol is already promoting some inflammation, made a noticeable difference in how I felt.
My anti-inflammatory timing:
- Omega-3 rich foods (wild salmon, walnuts) in the evening
- Avoid processed omega-6 oils during morning hours
- Use turmeric with black pepper and healthy fats for better absorption
The turmeric trick really works, by the way. Black pepper increases absorption by something like 2000%, and the healthy fats help too.

Rainbow Rotation Instead of Same Foods Every Day
Instead of eating the same antioxidant-rich foods every day, I started cycling through different colors and types. Monday might be blueberry day, Tuesday could focus on red bell peppers and tomatoes, Wednesday might feature orange sweet potatoes and carrots.
This “rainbow rotation” ensures you’re getting a wide spectrum of different antioxidants, each supporting different aspects of pregnancy health. Plus, it keeps meals interesting when your food preferences are changing daily.
My rainbow strategy:
- Different color focus each day
- Combine colorful foods with healthy fats for absorption
- Time consumption with natural energy dips for optimal use
The variety also helped with nausea – when I got tired of one color group, I could switch to another without abandoning antioxidants altogether.
Dealing With Stress Without Stressing About It
Stress-Supporting Foods That Actually Help
Pregnancy stress is real, and it can impact fetal development. Instead of just trying to eliminate stress (impossible), I focused on supporting my body’s ability to handle it through certain foods.
Holy basil tea with meals containing B-vitamins became my afternoon ritual. Combining stress-supporting foods with protein seemed to provide more sustained benefits than taking them alone.
My stress-support approach:
- Combine stress-supporting foods with magnesium-rich options
- Use holy basil tea with B-vitamin rich meals
- Pair stress-supporting foods with protein for sustained benefits
The key was consistency rather than intensity. Small, regular doses of stress support seeme d more effective than sporadic large amounts.
Recent expert guidance emphasizes that “pregnancy symptoms like vomiting, nausea, dizziness, and food aversion are observed. A curated diet plan is required to manage the symptoms”, which is why supporting your body’s stress response becomes even more important when you’re already dealing with first trimester challenges.
Eating for Two Without Actually Eating for Two
Your metabolism during pregnancy isn’t just “eating for two” – it’s learning to efficiently share resources between you and your baby. This requires a delicate balance that most pregnancy advice oversimplifies.
I had to unlearn a lot of pre-pregnancy habits and figure out how to maintain energy without doing anything that could harm my developing baby. It’s definitely a learning curve, and some days I got it right, other days I didn’t.

The Overnight Fasting Thing (It’s Not Scary, I Promise)
The whole “fasting while pregnant” thing probably sounds terrifying. I get it. But we’re literally just talking about not eating between dinner and breakfast – something you probably already do. I’d finish dinner around 7 and have breakfast around 7. Nothing dramatic, just letting my body do its thing overnight.
Full ketosis during pregnancy is a no-go, but mild ketone production? That can actually benefit your baby’s developing brain. A simple 12-hour gap between dinner and breakfast naturally produces these beneficial ketones.
My gentle overnight routine:
- Finish eating by 7 PM, break fast at 7 AM
- Make sure last meal has healthy fats and protein to sustain you
- Monitor energy levels and adjust timing if you’re feeling particularly drained
Some days I needed to shorten the window if I was feeling particularly exhausted. Pregnancy isn’t the time for rigid rules.
MCT Oil: My Secret Weapon (Start Small!)
MCT oil became my secret weapon for providing immediate ketones without the risks of full ketosis. But you have to start small – I learned this the hard way after a rather unpleasant digestive experience.
Starting with just half a teaspoon in my morning coffee and gradually working up to a tablespoon over two weeks made all the difference. Always consumed with other fats to prevent stomach upset.
My MCT approach:
- Start with 1/2 teaspoon MCT oil in morning coffee
- Gradually increase to 1 tablespoon over two weeks
- Always consume with other fats to prevent digestive upset
The sustained energy boost was noticeable, and I felt confident I was giving my baby’s brain an extra advantage during this critical development period.
Never Eating Carbs Alone
Never eating carbohydrates alone became my golden rule. Every carb needed a protein and fat buddy to prevent blood sugar spikes and crashes that could affect both me and baby.
I started using a rough 40-30-30 ratio (carbs-protein-fat) for main meals and paid attention to how different combinations affected my energy and nausea levels. Some combinations worked way better than others.
My blood sugar strategy:
- Never eat carbs alone – always pair with protein and fat
- Use a 40-30-30 ratio for main meals as a starting point
- Monitor how different combinations affect your energy and nausea
The personalization aspect was huge. What worked for my friend’s pregnancy didn’t necessarily work for mine, so I had to experiment and find my own optimal combinations.
| Meal Component | When I Had It | What I Paired It With | Why It Helped |
|---|---|---|---|
| Complex Carbs | Morning/Midday | Protein + Healthy Fat | Stable blood sugar |
| Lean Protein | Every meal | B-vitamins + Iron | Fetal development |
| Healthy Fats | Evening/Energy dips | Fat-soluble vitamins | Hormone production |
| Fiber | Throughout day | Adequate water | Digestive health |
Supporting Blood Sugar Without Obsessing
The Cinnamon Trick
Adding Ceylon cinnamon to chromium-rich foods became a simple way to support blood sugar stability. I’d sprinkle cinnamon on my oatmeal with nuts, or add it to roasted vegetables.
Having these combinations before higher-carb meals seemed to help with glucose management, though I was careful to track my response since every pregnancy is different.
My blood sugar support:
- Add Ceylon cinnamon to chromium-rich foods (broccoli, whole grains)
- Have these combinations before higher-carb meals
- Track how you feel if monitoring is recommended by your provider
The taste combinations were actually quite pleasant – cinnamon on roasted sweet potatoes became a regular favorite.
The Post-Meal Walk
A gentle 10-15 minute walk about 30 minutes after eating became my routine for glucose management. Not immediately after eating (that felt uncomfortable), but after things had settled a bit.
The key was keeping it gentle and rhythmic rather than intense. This wasn’t about burning calories – it was about helping my muscles take up glucose more efficiently.
My post-meal movement:
- Take a 10-15 minute gentle walk 30 minutes after eating
- Avoid vigorous movement immediately after meals
- Focus on steady, rhythmic movement rather than intensity
These walks also became a nice mental break and helped with digestion overall.

The Nutrient Combinations That Made a Real Difference
Beyond just hitting my daily targets for each vitamin and mineral, I learned that specific combinations create effects that are way better than taking things alone. Understanding these interactions completely changed my approach to meal planning.
I spent way too much time initially just focusing on getting enough of each nutrient. But learning about how they work together made a much bigger difference than I expected.
The Iron Absorption Puzzle
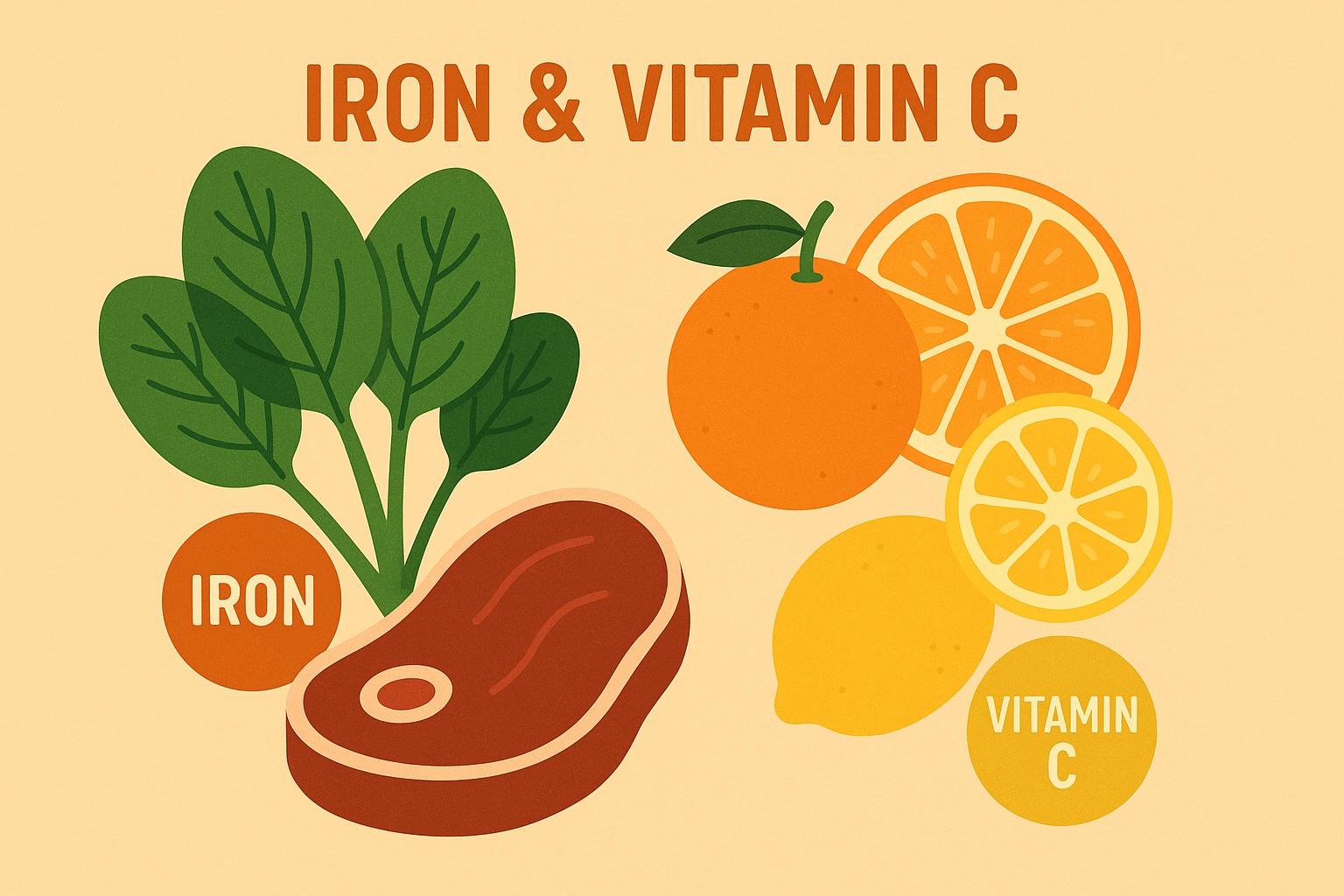
The daily iron requirement is 27mg daily according to RDA guidelines, but actually absorbing that iron requires understanding how it interacts with other nutrients.
Meat Iron vs. Plant Iron
All iron sources aren’t created equal, and I learned this lesson when my iron levels weren’t improving despite eating iron-rich foods. Iron from meat sources and iron from plants need completely different strategies.
Having meat-based iron during my morning energy peaks seemed to work better, while plant-based iron paired with vitamin C-rich foods in the afternoon was more effective. Separating iron-rich meals from calcium by at least two hours made a noticeable difference.
Understanding iron absorption becomes even more important when you consider that certain nutrient-dense foods can either enhance or inhibit mineral uptake depending on timing and combinations.
My iron strategy:
- Have meat-based iron sources during morning energy peaks
- Take plant-based iron with vitamin C-rich foods in afternoon
- Separate iron-rich meals from calcium-rich foods by 2+ hours
The timing aspect was something I’d never considered before, but it made sense once I understood how different hormones affect mineral absorption.
Jennifer, a mom I know, struggled with iron deficiency until she restructured her eating schedule: meat-based iron at breakfast (8 AM), and plant-based iron foods with strawberries at lunch (1 PM), while moving her calcium-rich yogurt snack to 4 PM. Her iron levels improved significantly within eight weeks.
The Copper Connection
Copper was the missing piece in my iron puzzle. Without adequate copper, your body can’t properly use iron, but too much copper during pregnancy can be problematic. Food sources became my safe middle ground.
Including copper-rich foods 2-3 times weekly, paired with iron-rich meals, seemed to help with iron utilization without overdoing it.
My copper balance approach:
- Include copper-rich foods (cashews, dark chocolate) 2-3 times weekly
- Pair with iron-rich meals for enhanced utilization
- Avoid copper supplements unless specifically recommended by your provider
The dark chocolate part wasn’t exactly a hardship – quality dark chocolate became my afternoon treat paired with iron-rich snacks.
The Calcium-Magnesium-Vitamin D Dance
Evening Magnesium for Better Sleep
Magnesium became my evening ritual. Absorption is better in the evening, and it also supports the deep sleep that’s crucial for growth hormone release during pregnancy.
Pumpkin seeds with dinner or a magnesium supplement 1-2 hours before bed, always with a small amount of healthy fat for absorption. The sleep improvement was immediate and noticeable.
My evening magnesium routine:
- Have magnesium-rich foods with dinner
- Take magnesium supplements 1-2 hours before bed
- Pair with small amounts of healthy fats for absorption
The better sleep quality had ripple effects throughout my pregnancy – more energy, better mood, less nausea.
Vitamin D Timing for Better Sleep
Vitamin D timing was something I’d never thought about, but it affects your sleep-wake cycles. Taking it with my morning meal containing fats, ideally within a couple hours of getting sunlight exposure, seemed to support better sleep patterns.
Avoiding vitamin D in the evening became important once I realized it could interfere with melatonin production and sleep quality.
My vitamin D routine:
- Take vitamin D supplements with morning meal containing fats
- Get sunlight exposure within 2 hours of vitamin D when possible
- Avoid vitamin D supplementation in evening hours
The combination of morning vitamin D and evening magnesium created a nice rhythm that supported both absorption and sleep.
Calcium: Less Is More (Per Meal)
Your body can only absorb about 500mg of calcium at a time, so splitting my intake across multiple meals became essential. I also learned that high-fiber meals can interfere with calcium absorption.
Pairing calcium sources with vitamin K2-rich foods created better utilization. It’s about getting calcium to where it needs to go, not just consuming enough.
My calcium approach:
- Split calcium intake across multiple meals (maximum 500mg per meal)
- Have calcium sources away from high-fiber meals
- Pair calcium with vitamin K2-rich foods for proper utilization
This approach required more planning but made a significant difference in how I felt and my lab results.

My First Trimester Nutrient Timing Checklist:
- Notice energy dips to identify when to have fat-soluble vitamins
- Try to get 20-25g complete protein within 30 minutes of waking
- Have prebiotic foods with dinner, fermented foods next morning
- Time omega-3 rich foods for evening
- Don’t eat between dinner and breakfast (12-hour window)
- Pair all carbs with protein and healthy fats
- Take vitamin D with morning meal containing fats
- Have magnesium 1-2 hours before bed
- Split calcium to maximum 500mg per meal
- Separate iron-rich meals from calcium by 2+ hours

Final Thoughts
Here’s what I want you to remember: I didn’t nail this stuff overnight. There were plenty of days when my “optimal nutrient timing” was a granola bar eaten while crying in my car. The strategies I’ve shared? They’re tools, not rules. Use what works, ditch what doesn’t, and give yourself grace for the days when none of it happens according to plan.
What surprised me most throughout this journey was how much control I actually had over my pregnancy experience through strategic eating. The nausea became manageable, my energy stabilized, and I felt confident that I was providing a good foundation for my baby’s development. But remember, every pregnancy is unique – what worked for me might need adjustment for your specific situation.
If reading all this makes you feel like you’re already behind or doing something wrong, take a deep breath. I felt the same way when I was researching all this stuff at 2 AM during my first trimester insomnia. You don’t need to implement everything at once. Pick one thing that sounds doable – maybe it’s just eating protein for breakfast or taking your vitamins with food instead of alone. Start there.
As you develop your personalized approach, consider exploring gut health strategies that can complement your nutrient timing and further support optimal absorption during this critical developmental window.
Also, can we acknowledge that not everyone has the luxury of perfectly timed meals? Some days my husband brought me whatever I could keep down, and we called it a win. If you’re working, dealing with other kids, or just trying to function through the fog of first trimester exhaustion, do what you can. Perfect is the enemy of good enough.
For additional support in managing first trimester challenges, explore natural immune support recipes that can be safely incorporated into your meal planning approach to maintain optimal health during this vulnerable period.
Now, before you start thinking you need to become a meal-timing ninja, let me tell you about the day I ate nothing but saltines and ginger ale until 3 PM. Sometimes pregnancy is just about survival, and that’s completely normal. Don’t try to overhaul everything at once – trust me, I learned this the hard way. Pick one small thing, like adding protein to your morning routine or taking your prenatal with dinner instead of on an empty stomach. Small changes add up.
The first trimester is challenging enough without adding pressure to be nutritionally perfect. Use these strategies as tools in your toolkit, not rigid rules to stress about. Your baby is incredibly resilient, and small, consistent improvements in your approach can have meaningful impacts on both your health and your child’s development.


