Your Acid Reflux Meal Plan Just Got a Major Upgrade (And It’s Not What You Think)


GERD affects about 20% of the population in the United States, making it one of the most common digestive disorders according to Oshi Health. If you’re part of this statistic, you’ve probably been handed the same generic list of foods to avoid – citrus, tomatoes, coffee, chocolate – while being told to eat bland, boring meals forever.
Look, I get it. I’ve been there – standing in the pharmacy aisle at 2 AM, desperately searching for something, anything, to stop that burning feeling in my chest. I used to be that person who carried Tums everywhere – in my purse, car, nightstand, you name it. I’d pop them like candy and wonder why I still felt like garbage. The worst part? Every doctor just handed me the same photocopied list of foods to avoid. No context, no explanation, just “don’t eat this stuff and deal with it.”
That’s when I realized I had to figure this out myself. After years of trial and error (and way too many sleepless nights), I finally discovered that everything we’ve been told about managing acid reflux through diet is missing the bigger picture. We’re focusing on what to eliminate instead of understanding how our bodies actually work.
Table of Contents
- Eating on Your Body’s Schedule
- Feeding Your Gut the Right Way
- Finding Your Personal Triggers
- Getting the Most Nutrition from Limited Foods
TL;DR
- Your stomach literally has its own schedule – timing meals strategically can reduce reflux episodes by up to 60%
- Those tiny bugs in your gut are actually running the show when it comes to acid production
- Generic trigger food lists don’t work because everyone’s reflux patterns are completely unique
- Your stomach can’t multitask – separating proteins and carbs can eliminate the need for many dietary restrictions
- Certain healing foods provide both therapeutic benefits and essential nutrients within reflux-friendly parameters
Eating on Your Body’s Schedule
Here’s something wild – your stomach literally has its own schedule, just like you do. It gets sleepy, it gets hyper, and it definitely has opinions about when you should be eating. Most people approach acid reflux backwards – they focus entirely on what foods to avoid instead of understanding when their digestive system naturally functions best.
This isn’t about eating bland foods forever. It’s about strategic timing that allows you to enjoy more variety with fewer consequences. Think of it this way: your stomach is like that coworker who’s super productive in the morning but completely useless after 3 PM. Work with it, not against it.
Recent research from Mass General Brigham highlights a global pattern in GERD prevalence that supports this timing approach. According to “When you look at map of the world that displays where people have more GERD, it tends to be areas where our diets are much more processed and lower in fiber or whole foods” Mass General Brigham reports. This geographical distribution suggests that our modern eating patterns – the timing and processing methods, not just food choices – are disrupting natural digestive rhythms.
Understanding Your Body’s Digestive Clock
Here’s the thing nobody talks about – your internal clock doesn’t just control when you sleep. It’s literally running every aspect of your digestion through a complex system of hormones and signals. Your stomach acid peaks in the evening while your digestive speed is strongest during daylight hours. Understanding these patterns creates natural windows where different types of meals work better.
I’ve found that most people experience their worst reflux symptoms because they’re fighting against their biology rather than working with it. When you align your eating schedule with your body’s natural digestive rhythm, you can often eat foods that previously caused problems.
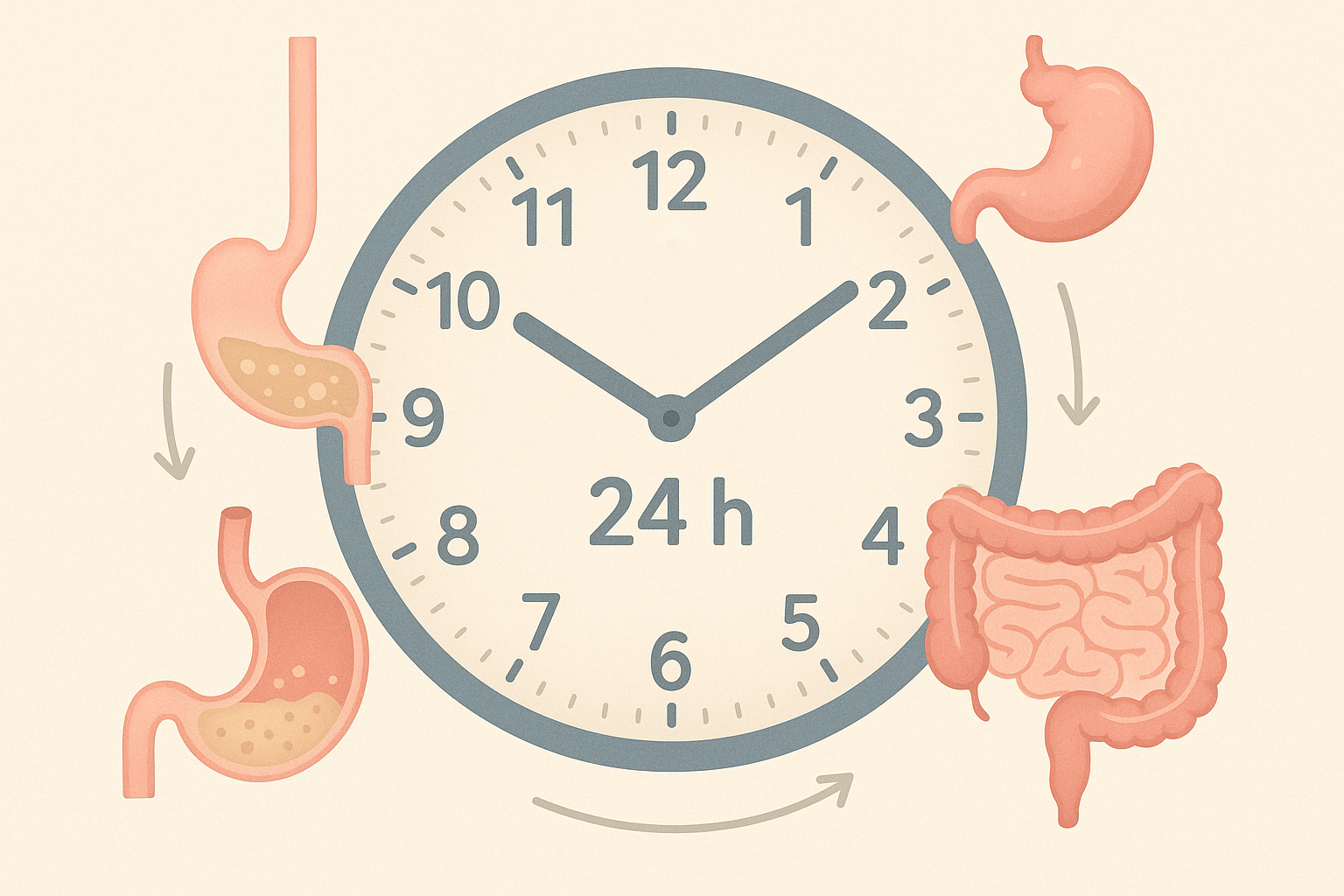
When Your Stomach Goes Into Overdrive
Your stomach acid follows a predictable 24-hour pattern, hitting rock bottom between 2-6 AM and surging from 6-10 PM. This means your evening meal strategy needs to be completely different from your morning approach. Instead of avoiding all acidic foods forever, you can actually use alkalizing foods strategically during peak acid hours to create natural balance.
Track when your symptoms hit hardest – I bet it aligns perfectly with these high-acid windows. Similar to how preparing oatmeal properly can maximize its digestive benefits, timing your meal components around your body’s natural acid production cycles creates optimal results.
Here’s how to actually do this:
- Pay attention to when your symptoms are worst throughout the day
- Schedule alkaline foods (leafy greens, melons, bananas) between 6-10 PM when acid naturally peaks
- Save neutral foods (oatmeal, rice) for morning hours when your stomach acid is naturally lower
| Time Window | What Your Stomach’s Doing | Best Food Choices | Skip These |
|---|---|---|---|
| 2-6 AM | Basically asleep | Light proteins, herbal teas | Large meals, caffeine |
| 6 AM-12 PM | Getting warmed up | Complex carbs, fruits | High-fat foods |
| 12-6 PM | Running at full speed | Balanced meals, vegetables | Spicy foods |
| 6-10 PM | Working overtime | Alkalizing foods, small portions | Acidic foods, large meals |
| 10 PM-2 AM | Winding down | Nothing (seriously, just stop eating) | All food and drink |
Why Your Stomach Empties Faster in the Morning
Your stomach empties fastest during morning and afternoon hours thanks to increased nerve activity and higher levels of hormones that speed up digestion. Evening digestion crawls along like traffic in rush hour, meaning food sits around longer and increases reflux risk.
This explains why that late dinner always comes back to haunt you at bedtime. The solution isn’t tiny portions everywhere – it’s strategic meal sizing based on your digestive speed.
Here’s how to actually do this:
- Front-load your largest meals before 3 PM when your digestive system runs at peak efficiency
- Keep evening meals under 400 calories to prevent overnight reflux episodes
- Include natural digestive boosters (ginger, artichokes) in afternoon meals to speed things up
In general, it’s recommended to stop eating at least 3 hours before you lie down or go to bed at night according to Season Health. This helps prevent backflow of acid into the esophagus and can reduce overnight reflux symptoms.
Real Example – Sarah’s New Schedule:
- 7 AM: Big breakfast (600 calories) – oatmeal with berries and nuts
- 12 PM: Substantial lunch (500 calories) – quinoa bowl with vegetables and lean protein
- 3 PM: Light snack (150 calories) – apple with almond butter
- 6 PM: Small dinner (350 calories) – steamed vegetables with small portion of fish
- After 8 PM: Only herbal tea or water
This schedule eliminated Sarah’s nighttime reflux episodes while letting her eat satisfying portions when her body could actually handle them.
Why Bedtime Reflux Happens (And It’s Not Your Fault)
Your lower esophageal sphincter naturally weakens during sleep preparation – it’s literally part of your body getting ready for rest. This biological process is completely normal, and fighting it creates more problems than solutions.
Instead of trying to force your sphincter to stay tight all evening, you can support its natural function and compensate for its evening relaxation through smart positioning and timing strategies.
Here’s how to actually do this:
- Stop eating 4 hours before bedtime to ensure your stomach is completely empty
- Try gentle yoga poses that support digestive function during early evening hours
- Sleep with your upper body slightly elevated to let gravity help compensate for natural sphincter relaxation

Why Your Stomach Can’t Multitask
Beyond timing, the actual makeup of your meals creates predictable digestive responses. Different types of food require completely different digestive environments, and forcing them together creates chaos in your stomach.
Your stomach can’t multitask any better than you can. Ask it to digest a steak AND a baked potato at the same time, and it’s going to throw a tantrum. That tantrum? That’s your heartburn. Just as improving digestion naturally requires understanding food combinations, creating an effective meal plan depends on strategic macronutrient pairing.
The Protein-Carb Separation Game Changer
Proteins need acidic conditions while carbohydrates prefer alkaline environments – combining them forces your digestive system into an impossible compromise. This creates the perfect storm for reflux symptoms.
I learned this the hard way when I kept getting reflux after my “healthy” grilled chicken and quinoa bowls. Turns out, my stomach was basically having a civil war trying to process both at once. Now I eat my protein with veggies at lunch and save the grains for dinner. Game changer.
Here’s how to actually do this:
- Separate protein and starch meals by at least 2 hours to avoid digestive conflicts
- Create protein-focused meals paired only with non-starchy vegetables
- Design carbohydrate meals around fruits, vegetables, and whole grains without animal proteins
Real Success Story:
Mark struggled with severe reflux whenever he ate chicken and rice together. By separating these foods, he now enjoys:
- Lunch: Grilled chicken with steamed broccoli and leafy green salad
- 3 PM: Small snack of nuts or seeds
- Dinner: Brown rice with roasted vegetables and avocado
This simple change eliminated 80% of his reflux episodes while allowing him to eat foods he thought were permanent triggers.
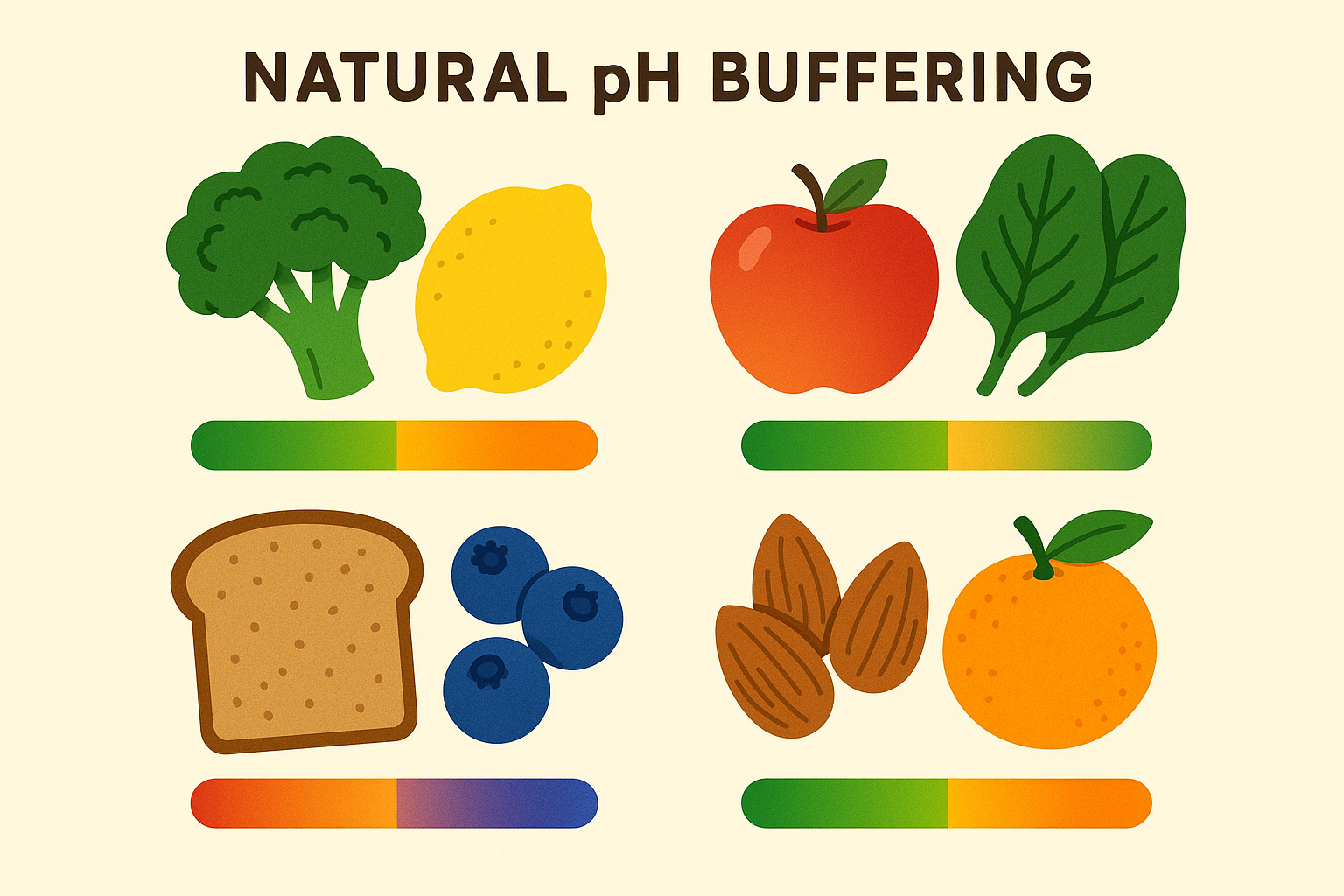
Creating Built-In Acid Neutralizers
Certain food combinations create natural buffering systems that neutralize excess stomach acid while maintaining optimal digestive function. These combinations work together instead of simply masking symptoms – they actually improve your digestive capacity over time.
The key is understanding which foods naturally complement each other’s pH levels and mineral content. This transforms your meal planning from a restrictive list into a strategic toolkit.
Here’s how to actually do this:
- Pair naturally acidic foods with alkalizers (tomatoes with fresh basil, citrus with leafy greens)
- Include mineral-rich foods (sea vegetables, raw nuts) to provide natural buffering compounds
- Create meals with built-in digestive enzymes (pineapple with protein, papaya with heavier foods)
Feeding Your Gut the Right Way
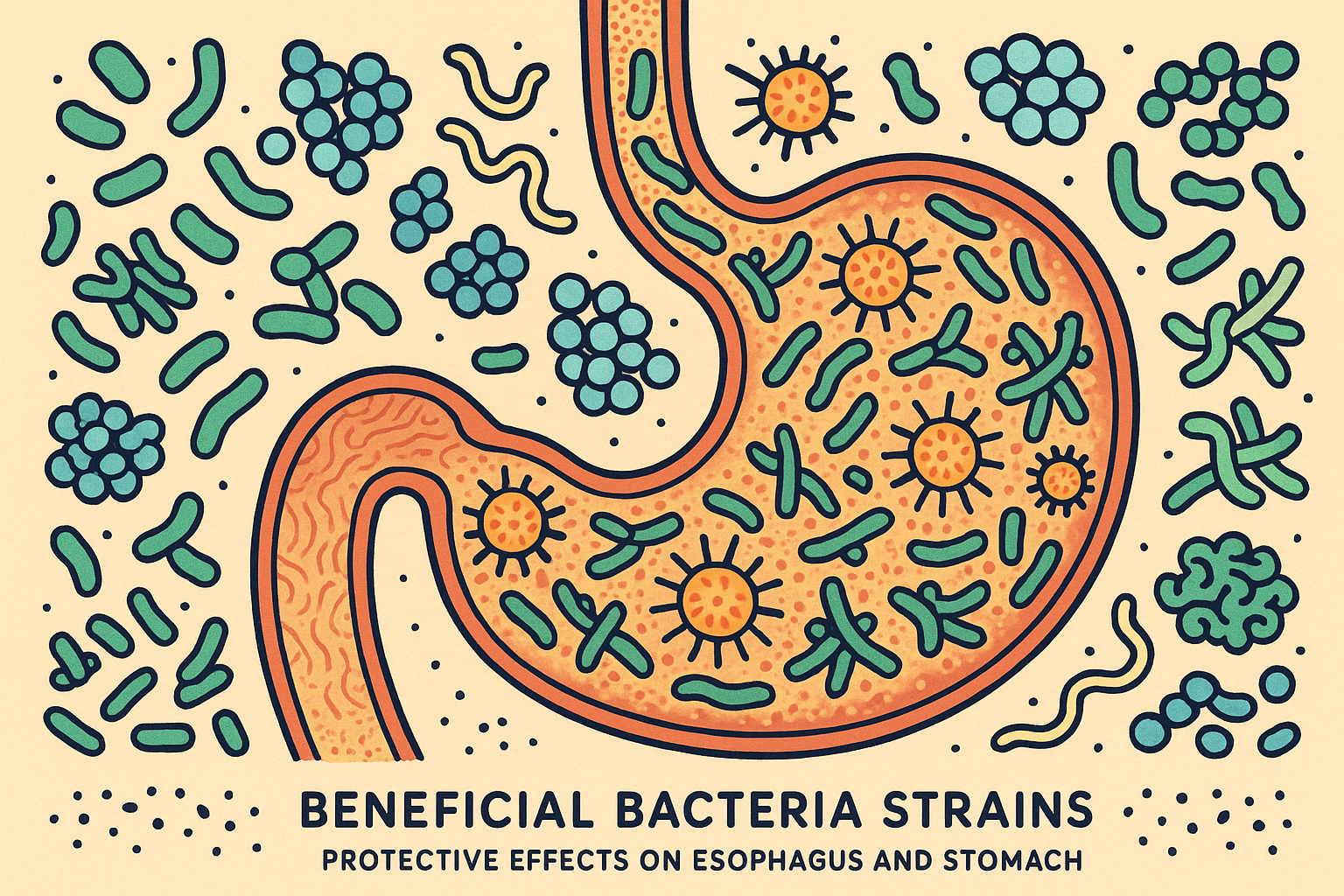
Those tiny bugs living in your gut? They’re not just freeloaders. They’re actually running the show when it comes to your digestion, controlling acid production, inflammation levels, and how well your digestive system functions. Most probiotic approaches are way too generic to address specific reflux mechanisms.
Your gut is basically a bustling city of tiny organisms, and some of them are actually your best friends when it comes to preventing heartburn. The trick is knowing how to keep the good guys happy. Understanding the connection between gut health and digestive disorders is essential, much like how drinking vinegars support gut health through beneficial bacterial cultivation in your meal planning approach.
Targeting the Right Bacteria for Reflux Relief
Different bacterial strains affect reflux through completely different mechanisms – some strengthen your esophageal barrier, others control acid production, and certain strains improve how fast your stomach empties. Generic probiotics are basically throwing darts blindfolded.
Targeting specific populations requires understanding which strains do what and how to cultivate them through food choices rather than just popping random supplements.
The H. Pylori Misunderstanding
Remember when everyone thought H. pylori was the villain? Turns out, it’s more like that friend who can be awesome or terrible depending on the crowd they’re hanging with. The medical world spent decades trying to eliminate it completely, but emerging research shows certain strains actually protect against reflux when present in balanced populations.
The goal isn’t to kick them out – it’s to make sure they’re bringing good vibes to the party. Complete elimination can sometimes make reflux worse.
Here’s how to actually do this:
- Test for H. pylori strain diversity rather than just presence or absence
- Include foods that support beneficial H. pylori strains (broccoli sprouts, green tea polyphenols)
- Avoid unnecessary antibiotic use that disrupts delicate bacterial balance
Your Esophageal Guardian: L. Reuteri
There’s this one bacterial strain called L. reuteri that produces specific compounds strengthening your esophageal lining and improving lower esophageal sphincter function – it’s basically a natural reflux medication produced by your own gut bacteria. This strain is particularly sensitive to modern dietary patterns and requires specific cultivation approaches.
Most people have depleted L. reuteri populations without realizing it, which directly contributes to reflux symptoms.
Here’s how to actually do this:
- Include L. reuteri-rich fermented foods (traditional sourdough, specific kefir strains)
- Provide prebiotic fibers that specifically feed L. reuteri (inulin, resistant starch from cooled potatoes)
- Eliminate foods that kill L. reuteri (processed sugars, artificial sweeteners)
The growing awareness of gut health’s role in digestive disorders has sparked interest in specialized diets. A recent article from VegNews discusses how “The bland diet is a short-term dietary intervention that focuses on foods that are gentle on the digestive system to allow the digestive system to rest and repair” VegNews reports. This approach aligns with microbiome restoration by reducing inflammatory triggers while beneficial bacteria populations recover.
Cooling the Inflammatory Fire
Chronic inflammation in your digestive tract perpetuates acid reflux through multiple pathways – it’s not just about acid levels. You know how your stomach gets all twisted up when you’re stressed? That inflammatory response is happening on a cellular level too, and it’s making everything worse.
Anti-inflammatory nutrition strategies can break this cycle by addressing root causes rather than just managing symptoms. This approach often allows people to reintroduce foods they thought they’d have to avoid forever.
Balancing Your Inflammatory Response
The modern diet’s skewed fatty acid ratio promotes inflammation throughout your digestive tract. Most people consume 15-20 times more omega-6 than omega-3 fatty acids, creating a pro-inflammatory environment that makes reflux symptoms worse.
Correcting this ratio reduces esophageal inflammation and dramatically improves healing capacity.
Here’s how to actually do this:
- Calculate your current omega-3 to omega-6 ratio through detailed food tracking
- Increase marine-based omega-3s while systematically reducing omega-6 cooking oils
- Include specialized inflammation-resolving foods like mackerel and sardines
Your Anti-Inflammatory Arsenal
Different plant compounds target specific inflammatory pathways involved in acid reflux. Maximizing variety provides comprehensive anti-inflammatory coverage that works better than any single compound.
The goal is variety, not quantity – your digestive system needs different compounds working together synergistically.
Here’s how to actually do this:
- Consume at least 30 different plant foods weekly to maximize anti-inflammatory variety
- Focus on deeply colored foods that indicate high compound content (purple cabbage, blueberries, dark chocolate)
- Include both water-soluble and fat-soluble compounds in each meal for comprehensive coverage

Finding Your Personal Triggers
Generic trigger food lists fail because everyone’s acid reflux patterns are completely unique based on genetics, lifestyle, stress patterns, and individual physiology. You probably already know when your symptoms are worst – you just haven’t connected all the dots yet.
I’ve seen people discover they can eat foods they avoided for years once they understand their individual patterns and optimal timing. Personalizing your approach is as important as understanding food allergies versus food intolerances when developing your customized meal plan.
Finding Your Real Triggers (It’s Not What You Think)
Most people think they know their trigger foods, but casual observation misses crucial variables. What looks like a food trigger might actually be a timing issue, stress response, or combination problem.
Look, I know tracking sounds like a pain, but hear me out. Start simple: jot down what you ate and how you felt a few hours later. You’ll start seeing patterns faster than you think.
Beyond the Obvious: What’s Really Causing Your Symptoms
True trigger identification requires tracking additional factors like sleep quality, stress levels, meal timing, and food combinations. That “tomato sensitivity” might actually be about eating tomatoes at 9 PM after a stressful day, not the tomatoes themselves.
Detailed analysis often reveals surprising patterns that completely change your dietary approach.
Here’s how to actually do this:
- Use detailed food and symptom journaling for at least 30 days to capture true patterns
- Track additional variables (sleep quality, stress levels, exercise timing, menstrual cycle)
- Look for patterns using correlation analysis to identify true triggers versus coincidental associations
Simple Tracking Checklist:
- ☐ Record exact time of each meal and snack
- ☐ Note portion sizes and how food was prepared
- ☐ Track stress levels (1-10 scale) before eating
- ☐ Document sleep quality from previous night
- ☐ Record symptom onset time and severity
- ☐ Note physical position during and after meals
- ☐ Track menstrual cycle phase (if applicable)
- ☐ Document exercise timing relative to meals
- ☐ Record weather patterns and seasonal changes
- ☐ Note medication timing and interactions
Your Digestive Blueprint: Why Genetics Matter
Some of us are built like race cars – we process everything fast. Others are more like reliable old trucks – slower but steady. There’s no right or wrong, just different. Once you figure out which one you are, everything else starts making sense.
Genetic variants significantly affect stomach acid production, enzyme function, and inflammatory responses. Understanding your genetic predispositions provides insights into optimal dietary approaches that work with your biology rather than against it.
Here’s how to actually do this:
- Consider genetic testing for variants affecting digestive function (particularly enzyme and inflammatory markers)
- Adjust meal planning based on genetic predispositions (slow vs. fast metabolizers need different approaches)
- Use genetic information to guide supplement choices and food preparation methods
Real Example – Genetic-Based Planning:
Lisa discovered through genetic testing that she has slow enzyme activity, meaning she metabolizes caffeine extremely slowly. Instead of eliminating coffee entirely, she now:
- Drinks one small cup only before 10 AM
- Chooses light roast over dark roast (lower caffeine)
- Pairs coffee with alkalizing foods like oat milk and cinnamon
- Avoids all caffeine after noon
This personalized approach eliminated her afternoon reflux episodes while preserving her morning coffee ritual.
Adapting to Life’s Changes
Your optimal management strategy will evolve based on life circumstances, seasonal changes, and physiological adaptations. What works in summer might not work in winter, and high-stress periods require different strategies than relaxed times.
Building flexibility into your approach ensures long-term success rather than rigid adherence to static rules.
Working With Natural Cycles
Ever notice how you crave different foods in winter versus summer? Your stomach notices too. In winter, when the sun sets at 4 PM, your body thinks it should be winding down for the day. Summer? You can get away with eating later because your internal clock is still running on daylight time.
Digestive function naturally varies with seasons due to circadian rhythm changes, activity levels, and food availability. Adapting your approach seasonally optimizes results and prevents the frustration of strategies that suddenly stop working.
Here’s how to actually do this:
- Adjust meal timing based on seasonal daylight patterns (earlier dinners in winter, later in summer)
- Incorporate seasonal foods that naturally support digestive function during each time of year
- Modify portion sizes and meal frequency based on seasonal activity levels and metabolic changes
| Season | Daylight Hours | Best Dinner Time | Supportive Foods | Activity Adjustments |
|---|---|---|---|---|
| Spring | Increasing | 6:00-6:30 PM | Fresh greens, sprouts, light proteins | Moderate exercise, outdoor activities |
| Summer | Peak | 6:30-7:00 PM | Cooling foods, raw vegetables, fruits | High activity, hydration focus |
| Fall | Decreasing | 5:30-6:00 PM | Root vegetables, warming spices | Moderate activity, stress management |
| Winter | Minimal | 5:00-5:30 PM | Warming foods, cooked vegetables | Low activity, comfort focus |

The Stress-Stomach Connection (It’s Real)
You know how your stomach gets all twisted up when you’re stressed? That’s not just in your head – it’s literally changing how much acid your stomach makes. Bad day at work equals bad night with heartburn. The connection is real, and ignoring it won’t make it go away.
High-stress periods require completely different meal planning approaches than relaxed times. Managing stress-related digestive issues requires understanding how your body stores tension and affects digestive function during challenging periods.
Here’s how to actually do this:
- Identify your personal stress patterns and their relationship to reflux symptom timing
- Plan lighter, easier-to-digest meals during predictably high-stress periods
- Include stress-reducing foods and mindful eating practices in your daily routine
Stress-Response Meal Planning:
- Low Stress Days: Normal portion sizes, can experiment with trigger foods, regular meal timing
- Moderate Stress Days: Smaller portions, stick to known safe foods, add calming herbal teas
- High Stress Days: Liquid/soft foods only, frequent small meals, focus on alkalizing foods
- Crisis Stress Days: Bone broth, herbal teas, minimal solid food, professional support if needed
Getting the Most Nutrition from Limited Foods
When you can’t eat half the foods on the planet, every bite needs to count. It’s like being on a budget – you’ve got to be smart about where you spend your “food dollars.” The good news? There are tricks to squeeze more nutrition out of the foods you CAN eat.
Managing acid reflux often requires eliminating many foods, which can lead to nutritional deficiencies if not carefully managed. Strategic food selection and preparation methods can dramatically increase nutrient density while remaining reflux-friendly.
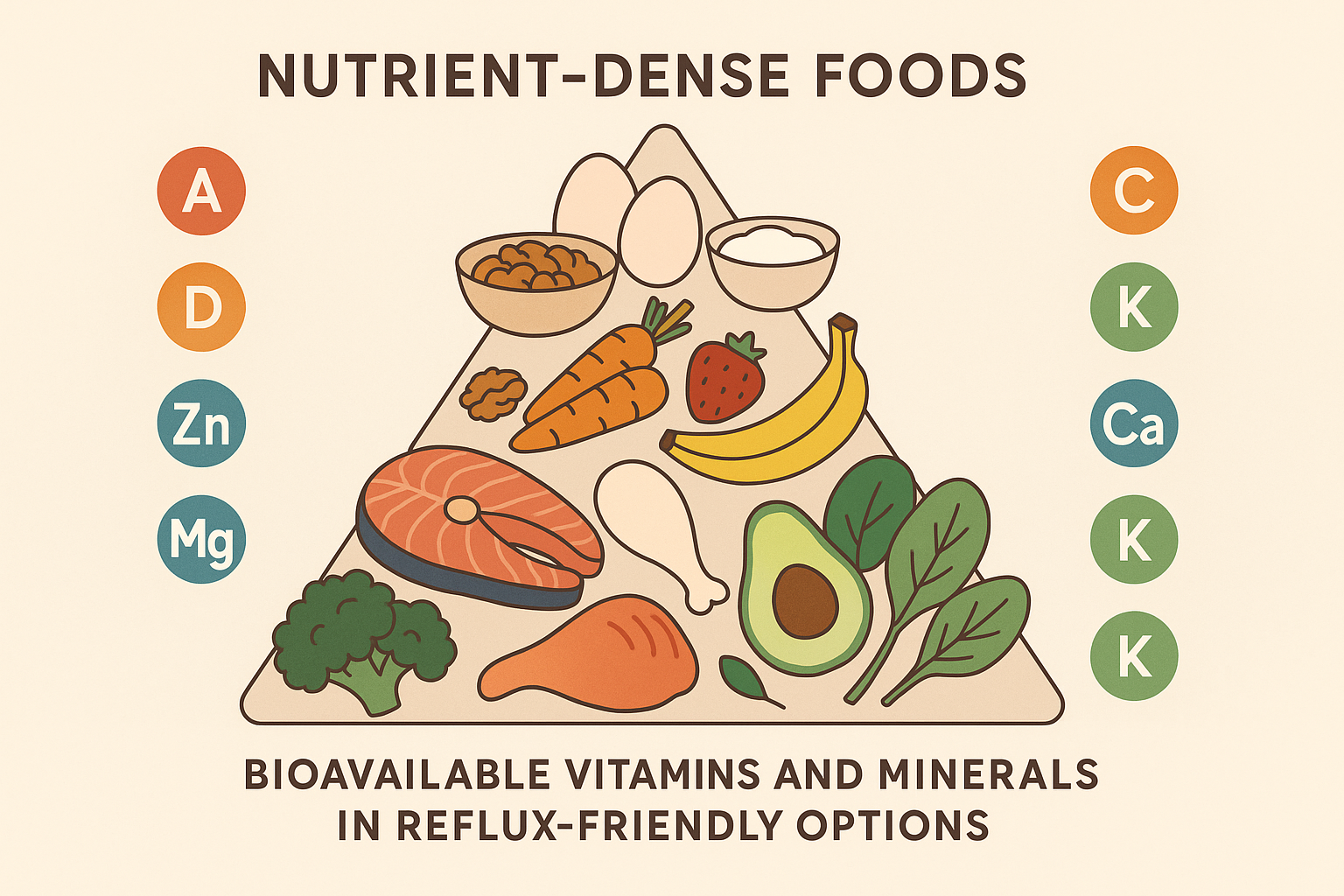
Making Every Nutrient Count
When food choices are limited, maximizing nutrient absorption becomes crucial. Raw nutrients on paper don’t always translate to absorbed nutrients in your body. Specific preparation and combination methods can dramatically increase how much nutrition you actually absorb from reflux-friendly foods.
Soaking your nuts overnight isn’t some fancy wellness trend – it actually makes them easier to digest and more nutritious. Same with lightly cooking your veggies instead of eating them raw. Sometimes your stomach needs a little help breaking things down.
Absorption Maximization Tricks
Fermentation, proper food combining, and strategic timing can turn nutritionally modest foods into powerhouses. Maximizing nutrient absorption is similar to understanding elimination diet principles – both require strategic approaches to optimize health outcomes within dietary restrictions.
Here’s how to actually do this:
- Use fermentation techniques to increase nutrient availability in vegetables (sauerkraut, kimchi)
- Combine vitamin C sources with iron-rich foods to enhance mineral absorption
- Include healthy fats with fat-soluble vitamins (A, D, E, K) for optimal uptake
Nutrient Absorption Maximization Checklist:
- ☐ Soak nuts and seeds overnight before eating
- ☐ Add lemon to iron-rich foods (when tolerated)
- ☐ Include good fats with every meal
- ☐ Chew thoroughly to increase surface area
- ☐ Eat fermented foods daily
- ☐ Time supplements with appropriate meals
- ☐ Cook vegetables lightly to break down cell walls
- ☐ Combine complementary proteins
- ☐ Avoid calcium with iron-rich meals
- ☐ Include digestive enzymes when needed
Foods That Heal While They Feed
Certain foods provide both nutritional value and specific therapeutic benefits for acid reflux, allowing you to address symptoms while meeting nutritional needs. These foods work as both medicine and nourishment, making them incredibly valuable when dietary options are limited.
Understanding which foods offer dual benefits helps you build a sustainable long-term approach.
Nature’s Digestive Soothers
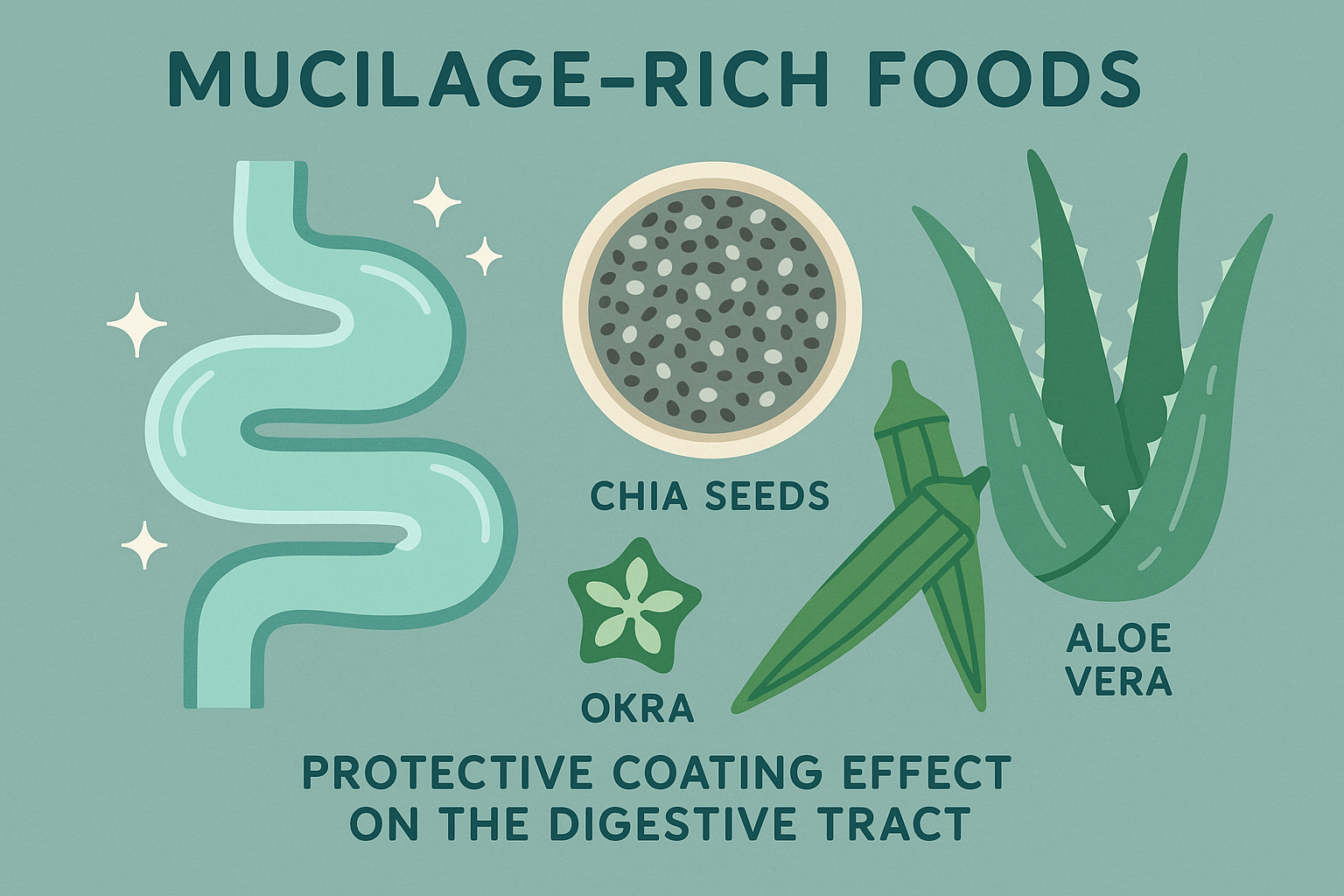
Foods containing natural mucilage compounds soothe and protect your digestive tract while providing essential nutrients. These foods create a protective coating that reduces acid contact with sensitive tissues while delivering vitamins, minerals, and fiber.
They’re particularly valuable because they’re both therapeutic and nutritious, serving double duty in restricted diets.
Here’s how to actually do this:
- Include okra, chia seeds, and marshmallow root in regular meal planning
- Prepare mucilage-rich foods properly to maximize therapeutic benefits (soaking chia, cooking okra correctly)
- Time consumption strategically for maximum protective effect (before potentially triggering meals)
Speaking of therapeutic nutrition, Organic Authority’s marine-sourced collagen offers superior bioavailability and a gentle, flavorless profile that makes it perfect for reflux-friendly meal plans. Its high-quality protein supports digestive healing while fitting seamlessly into the circadian rhythm and microbiome strategies we’ve discussed. Consider adding it to your morning routine when acid production is naturally lower.
Final Thoughts
Here’s what I want you to remember: this isn’t about perfection, and it’s definitely not about giving up everything you love forever. It’s about getting to know your body well enough to work with it instead of against it. Some days you’ll nail it, other days you’ll be reaching for the antacids – and that’s okay. Progress, not perfection.
Managing acid reflux doesn’t have to mean accepting a lifetime of bland, restrictive eating. Understanding your body’s natural rhythms, microbiome needs, and individual response patterns opens up possibilities you probably thought were off-limits forever.
The key is working with your biology rather than against it – timing meals strategically, supporting beneficial bacteria, and optimizing nutrient absorption within your personal parameters. This approach takes more initial effort than following generic trigger lists, but it creates lasting improvements that actually strengthen your digestive system over time.
Your meal plan should evolve with you, adapting to seasonal changes, stress levels, and life circumstances while maintaining the core principles that support optimal digestive function. Remember that developing a successful approach requires understanding that intuitive eating principles can complement your structured meal planning, helping you tune into your body’s unique responses and needs.


