Diabetic Meal Plan Secrets: Why When You Eat Matters More Than What You Eat

Table of Contents
- The Game-Changing Science Behind Meal Timing
- Your Body’s Hidden Glucose Patterns Throughout the Day
- Strategic Food Combinations That Actually Work
- Breaking Free from Emotional Eating Cycles
- Using Technology to Outsmart Your Metabolism
- Advanced Timing Tricks for Maximum Results
TL;DR
- Your body handles sugar best in the morning and worst at night – plan your biggest meals accordingly
- Mixing fiber, healthy fats, and protein in the right amounts can stop blood sugar from going crazy
- Stress hormones mess with your blood sugar big time, so managing emotions isn’t just nice-to-have
- Those continuous glucose monitors give you real-time feedback to figure out what actually works for you
- There’s a magic window after exercise where you can eat carbs without your blood sugar freaking out
- Poor sleep equals poor blood sugar control – it’s that simple
The Game-Changing Science Behind Meal Timing
For years, I obsessed over every carb and sugar gram, thinking that was the secret to managing my diabetes. You know the drill – no sugar, limit carbs, count everything like your life depends on it. Turns out, I was missing something huge: when you eat matters just as much as what you eat.
I’ll never forget the day I ate the exact same oatmeal breakfast at 8 AM versus 8 PM. Morning reading? A gentle 20-point rise. Evening? My blood sugar shot up 80 points! That’s when it clicked – my body was literally on a schedule I’d been ignoring for years.
Most diabetic meal plans focus exclusively on food restrictions, but here’s what blew my mind: your body’s internal clock doesn’t just control sleep – it runs the whole show when it comes to how you process sugar, make hormones, and handle glucose every single day.
Understanding these patterns transforms meal planning from guesswork into actually knowing what you’re doing. The American Diabetes Association emphasizes that effective diabetes meal planning requires understanding how different approaches work for individual needs, making personalized timing strategies essential for optimal glucose control.
Your Morning Metabolic Sweet Spot
Think of your morning metabolism like a hungry teenager – it’ll devour whatever you feed it and ask for more. Between 6-10 AM, your body operates in peak glucose-processing mode. Your body handles sugar best during these hours, meaning your muscles and liver eagerly soak up glucose instead of letting it hang out in your bloodstream causing trouble.
This biological advantage window makes morning the ideal time for your highest-carb meal of the day. Yeah, I know it sounds backwards if you’ve been trained to think carbs are the enemy, but hear me out.
You’ve been fasting all night, your stress hormones are naturally elevated (in a good way for once), and your cellular machinery is primed and ready to handle glucose. This is when you can actually enjoy those complex carbohydrates that might send your blood sugar to the moon later in the day.
Why Your Biggest Meal Should Happen Before 10 AM
During the early morning hours, your body’s like an efficient factory running at full capacity. Your natural stress hormones are doing their job – enhancing how well your body responds to insulin and cranking up your metabolic rate. Eating complex carbs during this window means you can enjoy foods that would normally make your glucose meter angry.
For those following a structured diabetic meal plan, understanding morning metabolism is crucial, especially when incorporating healthy breakfast foods that can support stable blood sugar levels throughout the day.
Sarah, a type 2 diabetic I know, discovered that eating her largest meal at 8 AM instead of 7 PM reduced her average daily glucose readings by 40 mg/dL. Her breakfast of steel-cut oats with berries and nuts caused a minimal 20 mg/dL spike, while the same exact meal at dinner previously spiked her glucose by 80 mg/dL. Same food, different time, completely different result.
Evening’s Metabolic Shutdown Mode
As daylight fades, your body begins preparing for rest by basically putting up a “closed” sign when it comes to processing carbs efficiently. This isn’t a bug in the system – it’s a feature that helped our ancestors store energy for overnight fasting. But for us diabetics? It means identical meals produce dramatically different glucose responses depending on when you eat them.
By evening, your body is more like a picky toddler who doesn’t want dinner and will throw a tantrum (aka blood sugar spike) if you force it to deal with too many carbs.
The 6 PM Carb Cutoff Strategy
Research consistently shows that your body’s ability to handle carbs crashes after 6 PM. Your declining insulin sensitivity, combined with rising melatonin production, creates a perfect storm for glucose spikes that’ll have you wondering why your morning numbers look like a phone number.
Limiting dinner carbs to under 30 grams and focusing on protein and healthy fats can prevent those frustrating bedtime blood sugar elevations. I’ve seen this strategy work wonders for people who were struggling with morning glucose readings – myself included.
| Time of Day | How Well Your Body Handles Sugar | Recommended Carbs | What to Focus On |
|---|---|---|---|
| 6-10 AM | Best (100%) | 45-60g | Complex carbs, protein |
| 10 AM-2 PM | Pretty Good (80%) | 30-45g | Balanced everything |
| 2-6 PM | Okay (60%) | 15-30g | Protein, healthy fats |
| After 6 PM | Not Great (40%) | Under 15g | Protein, vegetables |
Personalizing Your Meal Frequency
Here’s where I’m going to break some conventional wisdom: the “eat six small meals a day” advice doesn’t work for everyone. I know, I know – it’s diabetes gospel. But your optimal eating pattern should match your individual glucose response patterns, lifestyle demands, and how flexible your metabolism actually is.
Some diabetics thrive on intermittent fasting, while others need consistent fuel every few hours to keep their blood sugar from going on a rollercoaster ride. The key is figuring out which camp you’re in.
Making Intermittent Fasting Work for Diabetics
Controlled fasting periods can reset how well your body responds to insulin and reduce overall glucose ups and downs, but they require careful implementation. You can’t just decide to stop eating for 16 hours and hope for the best – trust me, I tried.
Starting with a 12-hour eating window and gradually extending it allows your body to adapt while you monitor glucose responses. It’s like training for a marathon – you don’t start with 26 miles on day one.
When considering intermittent fasting as part of your diabetic diet, it’s important to understand how women can safely approach intermittent fasting while maintaining stable glucose levels and adequate nutrition.
The key is breaking fasts with protein and healthy fats rather than carbohydrates to prevent rebound spikes. I’ve found that starting your eating window with eggs and avocado works much better than jumping straight into oatmeal or fruit. Learn from my mistakes – don’t break a 16-hour fast with a banana. Just don’t.
Recent medical guidance from Medscape emphasizes that intermittent fasting can be beneficial for motivated diabetic patients who regularly monitor blood sugars and understand medication adjustments. However, doctors stress the importance of adequate protein intake and careful monitoring to prevent hypoglycemia, especially for patients on insulin or sulfonylureas.

The Micro-Meal Approach for Severe Insulin Resistance
If your insulin resistance is severe and your blood sugar acts like a moody teenager no matter what you do, eating smaller portions every 2-3 hours can prevent the glucose rollercoaster while keeping your energy steady. This strategy requires dividing your daily food needs into six equal portions and sticking to consistent timing intervals.
Here’s my lazy person’s guide to micro-meals (because who has time to be perfect?):
Micro-Meal Planning Made Simple:
- Figure out how much you need to eat in a day (yeah, I know, math)
- Divide it into 6 tiny meals (think snack-sized portions)
- Set your phone to bug you every 2.5 hours
- Prep everything on Sunday so you’re not scrambling
- Track your blood sugar response for 2 weeks
- Adjust portion sizes based on what your meter tells you
- Pay attention to your energy levels throughout the day
Phone alerts help maintain consistency until the pattern becomes automatic. I recommend setting them for every 2.5 hours initially, then adjusting based on your glucose responses. Fair warning: you’ll feel like you’re constantly eating at first, but your blood sugar will thank you.
Seasonal Adjustments Your Body Craves
Your metabolic needs shift with the seasons due to changes in daylight exposure, temperature, and natural rhythm variations. Winter’s reduced sunlight can mess with your internal clock and increase insulin resistance, requiring modifications to your standard meal timing and composition.
During darker months, you might need to eat your largest meal even earlier – around 7 AM instead of 9 AM – to compensate for the disrupted signals your body is getting. Have you noticed your glucose control getting trickier during winter months? You’re not imagining it.
I used to think I was just more stressed during the holidays, but it turns out my body was literally confused by the lack of sunlight. Once I started adjusting my meal timing seasonally, winter became much more manageable.
Your Body’s Hidden Glucose Patterns Throughout the Day
Beyond basic meal timing, your body creates specific windows throughout each day that offer unique opportunities for strategic eating. Understanding these patterns allows you to work with your biology rather than constantly fighting against it, turning your natural rhythms into powerful tools for glucose management.
It’s like learning the secret handshake your metabolism has been waiting for all along.
The Post-Exercise Glucose Gateway
Physical activity creates a temporary state where your muscles can absorb glucose without requiring much insulin help. This 30-120 minute window after exercise offers diabetics a rare opportunity to consume carbohydrates with minimal blood sugar impact, essentially bypassing normal glucose control mechanisms.
It’s like having a VIP pass to eat carbs without the usual consequences. But like any VIP pass, the window doesn’t stay open forever.

Timing Your Post-Workout Fuel
During the immediate post-exercise period, your muscles act like glucose sponges, rapidly absorbing available carbs to replenish depleted energy stores. Consuming 15-30 grams of simple carbohydrates within 30 minutes post-workout, paired with 10-15 grams of protein, can actually improve recovery while maintaining glucose control.
This is one of the few times I tell diabetics they can have that banana or those dates without worrying too much about the glucose spike. Your muscles are literally crying out for fuel, and they’ll grab it before it has a chance to elevate your blood sugar.
But don’t go crazy – this isn’t a free pass to eat a whole pizza. We’re talking strategic refueling, not a carb festival.
Matching Nutrition to Exercise Type
Different types of physical activity create distinct metabolic demands requiring tailored nutrition strategies. Resistance training increases protein needs for muscle recovery, while high-intensity intervals can cause delayed glucose elevation 4-6 hours later (yeah, that’s a fun surprise). Tracking these patterns over several weeks reveals your personal exercise-glucose relationship.
| Exercise Type | Duration | Post-Workout Carbs | Post-Workout Protein | Timing Window |
|---|---|---|---|---|
| Walking | 30-60 min | 10-15g | 5-10g | Within 60 min |
| Resistance Training | 45-60 min | 20-30g | 15-20g | Within 30 min |
| High-Intensity Intervals | 20-30 min | 15-25g | 10-15g | Within 45 min |
| Swimming | 45-90 min | 25-35g | 15-25g | Within 30 min |
Sleep’s Secret Role in Glucose Control
Poor sleep quality directly messes with glucose metabolism and insulin sensitivity, creating a vicious cycle where high blood sugar disrupts sleep, which then makes glucose control worse the following day. Strategic evening nutrition can break this cycle by supporting both sleep quality and overnight glucose stability.
I can’t stress this enough – if you’re not sleeping well, your glucose control will suffer no matter how perfect your meal timing is during the day. It’s like trying to drive a car with flat tires – you might get where you’re going, but it’s going to be a bumpy ride.
Pre-Sleep Nutrition That Actually Helps
Including foods rich in tryptophan 2-3 hours before bed supports natural melatonin production while providing steady amino acids for overnight muscle maintenance. Think turkey, but also eggs, cheese, and nuts – not just Thanksgiving dinner.
Understanding how to boost your immune system through proper nutrition can also support better sleep patterns and glucose control.
A small protein snack can also prevent the dawn phenomenon – that frustrating morning glucose spike that occurs even when you haven’t eaten since dinner. It’s like your liver decides to throw a party at 4 AM and forgot to invite you.
Mark struggled with dawn phenomenon until he started eating 1 ounce of almonds with a small piece of cheese 2 hours before bed. This simple change reduced his morning glucose spikes from 180 mg/dL to 140 mg/dL within three weeks, while also improving his sleep quality scores on his fitness tracker. Sometimes the simplest solutions are the most effective.
Strategic Food Combinations That Actually Work
Moving beyond simple carb counting (which, let’s be honest, gets old fast), specific nutrient combinations create effects that can dramatically reduce post-meal glucose spikes. These food pairings work through multiple pathways in your body, offering more powerful glucose control than any single food could achieve alone.
It’s like assembling a superhero team for your blood sugar – each member has their own powers, but together they’re unstoppable.
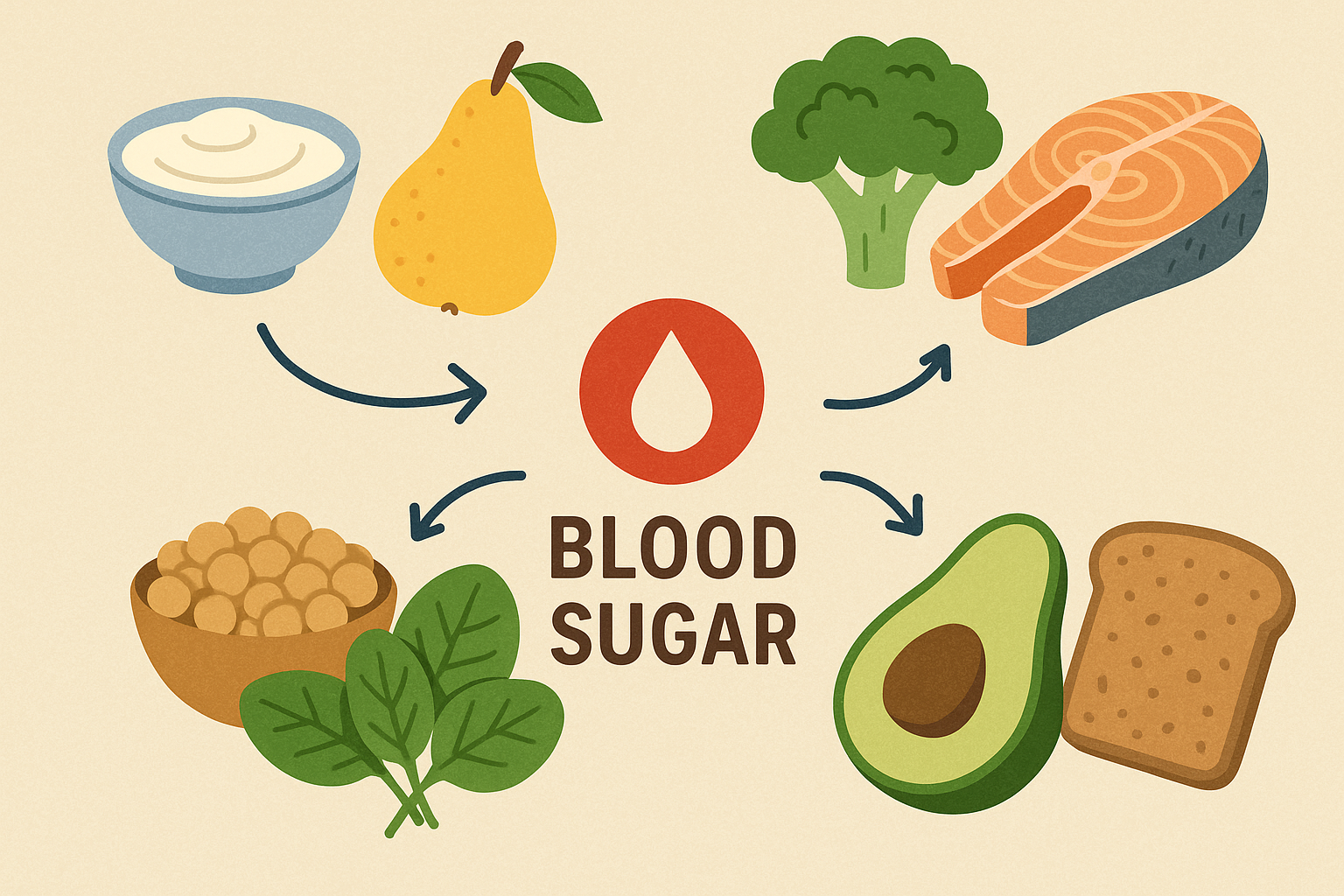
The Fiber-Fat-Protein Power Trio
Combining soluble fiber, healthy fats, and complete proteins in specific ratios creates a glucose-stabilizing effect that’s greater than the sum of its parts. This combination slows down how fast your stomach empties, reduces glucose absorption speed, and provides sustained fullness that prevents between-meal blood sugar swings.
Understanding the importance of fiber in your diabetic diet goes beyond just blood sugar control – fiber provides numerous health benefits including improved digestion and cardiovascular health.
Think of it as building a traffic control system for your digestive tract – everything moves more smoothly and at a manageable pace.
Getting the Ratios Right
Aim for approximately 10 grams of fiber, 15 grams of healthy fats, and 25 grams of protein per main meal. The sequence matters too – consuming fiber sources first, followed by protein, then any carbohydrates can further blunt glucose responses.
Adding 1-2 tablespoons of apple cider vinegar 15 minutes before carb-containing meals provides additional glucose-blunting benefits. I know it sounds weird and tastes like punishment, but the science backs this up. Chase it with water – trust me on this one.
Perfect Ratio Meal Planning Template:
- Fiber (10g): 1 cup broccoli + 1/2 avocado
- Healthy Fats (15g): 2 tbsp olive oil or nuts
- Protein (25g): 3.5 oz chicken breast or fish
- Optional Carbs: 1/3 cup quinoa or sweet potato – Timing: Eat fiber first, protein second, carbs last
Plant Compounds That Block Glucose Absorption
Natural compounds found in berries, green tea, and cinnamon can actually block some glucose absorption in your intestines while improving how well your cells respond to insulin. These natural compounds work as mild, food-based medications when consumed strategically with meals.
It’s like having tiny bouncers in your digestive system that slow down the sugar rush.
Timing Your Natural Glucose-Blockers
Drinking one cup of green tea 30 minutes before meals provides optimal concentrations of these helpful compounds right when glucose absorption begins. Adding one teaspoon of Ceylon cinnamon to morning meals or including a handful of berries with carb-containing meals maximizes these glucose-blocking effects.
The key word here is Ceylon cinnamon – not the regular stuff you find at most grocery stores. Ceylon cinnamon contains higher concentrations of the active compounds that actually help with glucose control. Yes, it’s more expensive, but your blood sugar meter will notice the difference.
Fixing the Nutrient Deficiencies That Worsen Diabetes
Diabetics commonly develop specific nutrient deficiencies that create a vicious cycle of worsening glucose control. Increased urinary losses of key minerals such as magnesium and chromium, combined with dietary restrictions, can impair insulin function and glucose metabolism.
It’s like trying to run a car on empty – eventually, something’s going to break down.
The Magnesium-Chromium Connection
These minerals directly influence how well your insulin receptors work and how your body processes glucose, yet deficiencies are extremely common in diabetic individuals. Including magnesium-rich foods daily, along with chromium sources, can gradually restore optimal levels and improve glucose control.
Pumpkin seeds, dark chocolate (yes, really), and leafy greens provide magnesium, while broccoli and whole grains supply chromium. I recommend tracking your intake for a week to see if you’re getting enough of these crucial minerals. Spoiler alert: you’re probably not.
According to recent guidance from Pancreatic Cancer Action Network, diabetic-friendly nutrition should focus on complex carbohydrates, plant-based foods with fiber, and high-protein foods with healthy fats at each meal. They emphasize eating meals at consistent times daily and including foods from each food group to maintain stable blood sugar levels.
Breaking Free from Emotional Eating Cycles
The psychological aspects of eating significantly impact glucose control through stress hormones, behavioral patterns, and long-term adherence to meal plans. Chronic stress elevates cortisol levels, which directly increases blood glucose and creates insulin resistance, making emotional management a crucial but often overlooked component of diabetic nutrition.
Look, I’m not going to pretend you’ll nail this perfectly. I’ve eaten gas station hot dogs at midnight and lived to tell about it. The goal isn’t perfection – it’s progress.

Understanding Your Stress-Glucose Connection
When you’re stressed, your body releases cortisol and adrenaline – hormones designed to provide quick energy for “fight or flight” situations. In modern life, this means chronic stress keeps your blood sugar elevated even when you haven’t eaten anything. Managing stress becomes as important as managing carbohydrates.
Managing stress is essential for blood sugar control, and understanding where your body stores tension can reveal important insights about your emotional health patterns that may be affecting your glucose levels.
Have you ever noticed your glucose readings spike during particularly stressful periods at work or home? That’s your stress hormones at work, and it’s completely normal. Your body doesn’t know the difference between a saber-toothed tiger and your boss – it just knows you’re stressed.
Mindful Eating as Medicine
Practicing mindful eating techniques can reduce stress-induced glucose spikes while improving your awareness of hunger and fullness signals. Eating without electronic distractions, chewing each bite 20-30 times, and taking three deep breaths before meals activates your body’s “rest and digest” mode, which supports better digestion and glucose control.
Mindful Eating Practice (The Non-Woo-Woo Version):
- Put your phone in another room (I know, it’s scary)
- Take 3 deep breaths before starting your meal
- Chew each bite 20-30 times (yes, count them at first)
- Put your fork down between bites
- Actually taste your food instead of inhaling it
- Check if you’re still hungry halfway through
- Stop eating when you’re 80% full (not stuffed)
Identifying Your Emotional Eating Triggers
Understanding your personal emotional eating patterns allows for proactive glucose management during high-stress periods. Keeping a mood-food journal for two weeks reveals connections between emotions and food choices that you might not consciously recognize.
Once you identify your top three triggers, you can develop non-food coping strategies and create emergency low-carb snack kits for challenging moments. I keep pre-portioned nuts and string cheese in my desk drawer for those afternoon stress moments when the vending machine starts calling my name.
Jennifer discovered through mood tracking that work deadlines triggered her afternoon cookie binges, spiking her glucose to 220 mg/dL. She replaced desk cookies with pre-portioned almonds and herbal tea, reducing stress-eating episodes by 80% and keeping afternoon glucose below 160 mg/dL. Sometimes awareness is half the battle.
Navigating Social Eating Without Sabotaging Your Health
Social situations often derail diabetic meal plans, but strategic preparation and communication can maintain glucose control while preserving relationships. The key is planning ahead rather than trying to make healthy choices in the moment when social pressure and limited options create perfect storms for poor decisions.
Had a stressful day and stress-ate a sleeve of crackers? Join the club. Tomorrow’s a new day, and your body is more forgiving than you think.
Restaurant Survival Strategies
Restaurant survival isn’t about being the difficult customer – it’s about being smart. Reviewing restaurant menus online beforehand (usually while procrastinating on something else), eating a small protein snack one hour before going, and requesting modifications can keep you on track without drawing unwanted attention to your dietary needs.
Most servers are happy to substitute vegetables for starches or bring dressing on the side. You don’t need to announce your diabetes to the entire table – just make your requests confidently. I’ve learned that “I’m trying to eat lighter” works better than a medical explanation.

Using Technology to Outsmart Your Metabolism
Getting a continuous glucose monitor was like having a brutally honest friend attached to my arm. It didn’t sugarcoat anything (pun intended). Some days it made me want to throw my phone across the room, but it taught me things about my body I never would have figured out otherwise.
Modern continuous glucose monitoring technology allows for real-time feedback and data-driven meal plan adjustments, moving beyond static meal plans to dynamic, responsive nutrition strategies. This technology transforms diabetes management from guesswork into actually knowing what works for your unique body.
Making Sense of Your Glucose Data
Learning to interpret continuous glucose monitor data helps identify which foods, combinations, and timing strategies work best for your unique metabolism. Rather than reacting to single readings (which will drive you crazy), focus on patterns and trends that emerge over time to make informed adjustments to your meal plan.
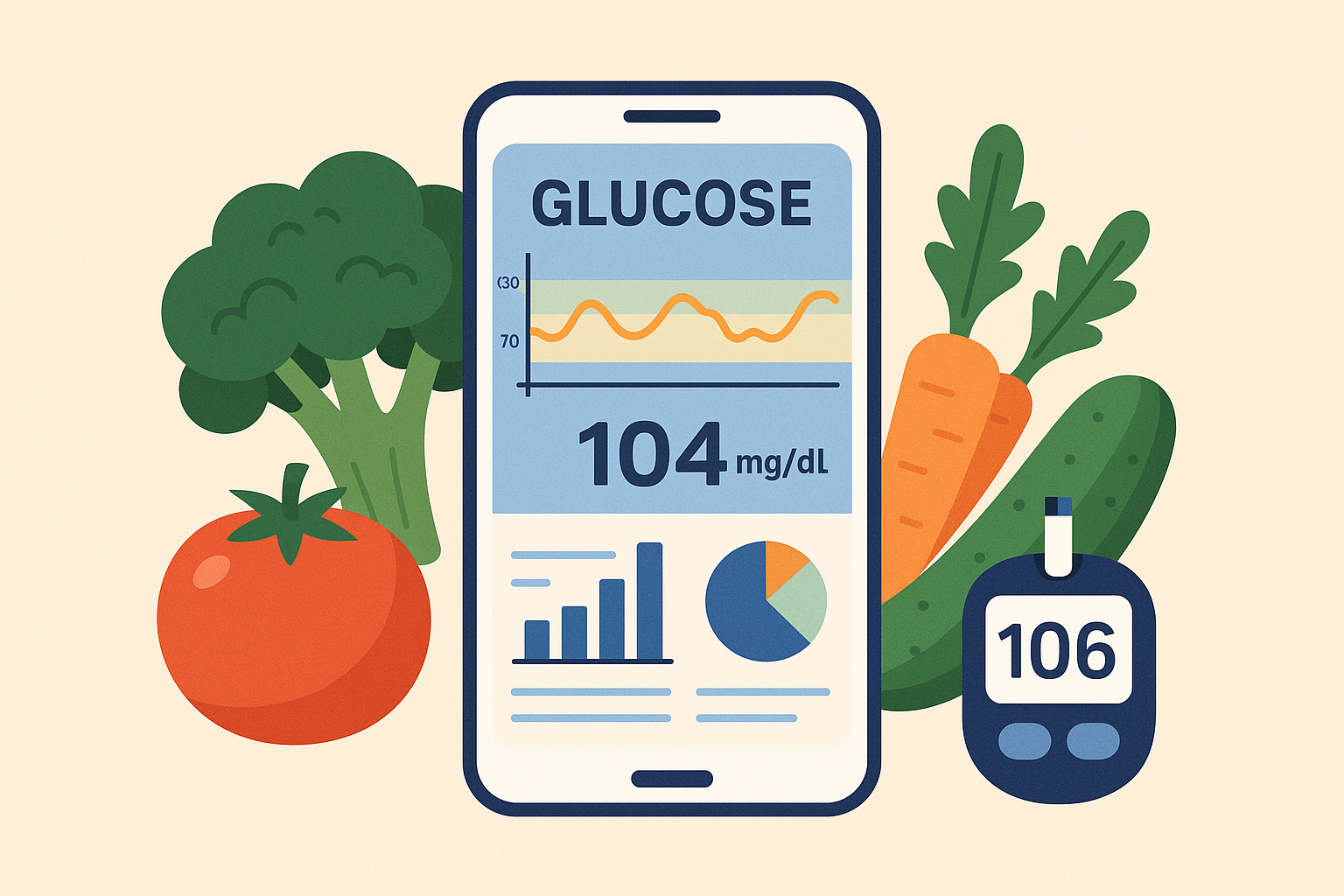
Pattern Recognition That Actually Matters
Track glucose responses to identical meals eaten at different times to understand your personal body clock patterns. Identify your threshold foods – those that consistently spike your glucose regardless of timing or combinations. We all have them.
Note connections between sleep quality and morning glucose levels, as poor sleep can elevate fasting glucose for 24-48 hours. I’ve found that even one night of poor sleep can throw off my glucose control for the next two days. It’s like my body holds grudges.
Coordinating Exercise and Nutrition for Maximum Impact
Monitoring your glucose response to pre-workout versus post-workout meals reveals optimal timing strategies for your lifestyle and exercise preferences.
Finding Your Exercise-Meal Sweet Spot
Timing moderate exercise 1-2 hours after your largest meals can significantly blunt glucose spikes while improving insulin sensitivity for the following meal. Post-meal walks are particularly effective and accessible for most people – even a 10-minute stroll helps.
Adjusting carbohydrate intake based on planned activity levels prevents both low blood sugar during exercise and excessive glucose elevation afterward. On days when I know I’ll be sedentary (hello, Netflix marathon), I automatically reduce my carb portions by about 25%.
Advanced Timing Tricks for Maximum Results
Beyond basic timing principles, specific windows throughout the day create opportunities for strategic nutrient delivery that can dramatically improve glucose control. These advanced strategies require more attention to detail but offer significantly better results for those willing to implement them consistently.
I know all this timing stuff sounds like a lot of work. But here’s the thing – once you get the hang of it, it actually makes life easier. No more guessing why your numbers are wonky. No more feeling like your body is working against you.
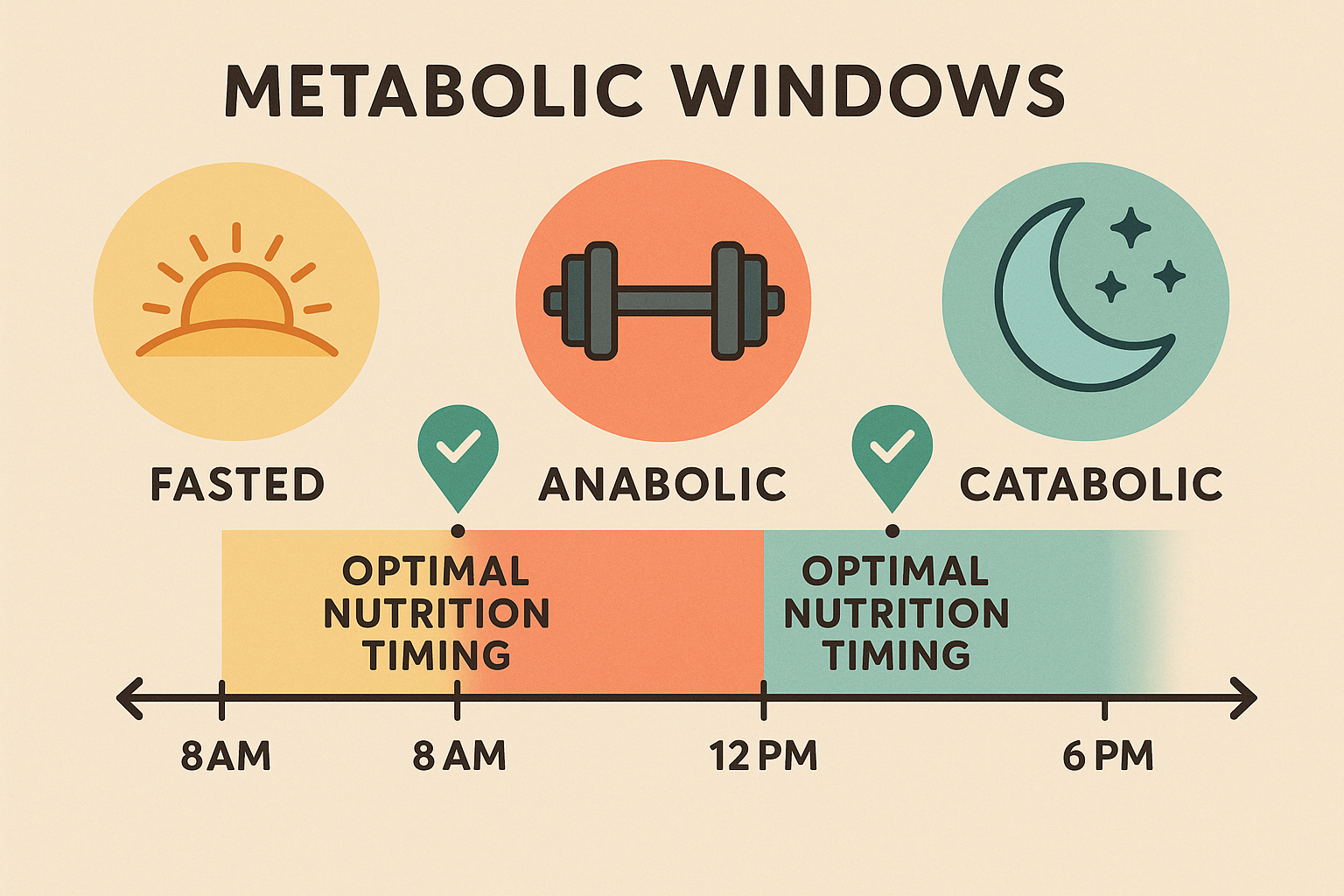
The Post-Exercise Carb Window Explained
The 30-120 minute period following physical activity creates unique metabolic conditions where glucose uptake occurs independently of insulin. During this window, your muscles can absorb glucose rapidly, offering diabetics a powerful tool for enjoying foods that might otherwise spike blood sugar.
Maximizing Your Recovery Strategy
Consuming 15-30 grams of simple carbohydrates within 30 minutes post-exercise, paired with 10-15 grams of protein, takes advantage of enhanced muscle glucose uptake while supporting recovery. This window allows you to consume foods typically restricted in your meal plan with minimal blood sugar impact.
Tailoring Nutrition to Your Exercise Type
Different types of physical activity create distinct metabolic demands requiring specific nutrition strategies. Resistance training increases protein needs for muscle recovery, while high-intensity intervals can cause delayed glucose elevation 4-6 hours later. Cardio sessions require focus on electrolyte replacement and moderate carbohydrates.
Post-Exercise Nutrition Protocol:
- Immediate (0-30 min): Simple carbs + fast protein
- Recovery (30-120 min): Complex carbs + complete protein
- Extended (2-4 hours): Monitor for delayed glucose response
- Hydration: Electrolyte replacement throughout
- Sleep: Extra protein if evening workout
Sleep Quality’s Hidden Impact on Glucose Control
Poor sleep quality directly impairs glucose metabolism and insulin sensitivity, creating a cycle where high blood sugar disrupts sleep, which then worsens glucose control the following day. Strategic evening nutrition can break this cycle by supporting both sleep quality and overnight glucose stability.

Pre-Sleep Nutrition Protocols That Work
Including tryptophan-rich foods 2-3 hours before bed supports natural melatonin production while providing steady amino acids for overnight muscle maintenance. Understanding how to boost your immune system through proper nutrition can also support better sleep patterns and glucose control.
Avoiding caffeine after 2 PM and limiting blue light exposure one hour before bedtime further supports healthy sleep patterns and glucose control.
For those experiencing dawn phenomenon – that frustrating morning glucose spike – a small protein snack before bed can provide steady amino acids that help prevent overnight glucose elevation. However, this strategy requires individual testing to ensure it doesn’t disrupt sleep quality.
The first time I tried eating my biggest meal at breakfast, I felt like I was going to explode. I’m talking Thanksgiving-dinner-level stuffed at 8 AM. Turns out, you don’t have to go from zero to hero overnight. Start with just making breakfast 25% bigger and dinner 25% smaller.

Final Thoughts
Listen, if you take nothing else from this novel I just wrote, remember this: your diabetes doesn’t define you, and you don’t have to be perfect. Managing diabetes through meal planning doesn’t have to feel overwhelming or restrictive. When you understand how your metabolism actually works throughout the day, you can make strategic choices that work with your biology rather than constantly fighting against it.
The most important takeaway? Start with one small change – maybe just moving your biggest meal earlier – and see how it feels. Maybe begin by timing your largest meal earlier in the day, or experiment with that fiber-fat-protein combination at dinner. Small, consistent changes create lasting results without overwhelming your daily routine.
Remember that your glucose patterns are as unique as your fingerprint. What works perfectly for someone else might need adjustment for your lifestyle, work schedule, and individual metabolism. Use continuous glucose monitoring data when possible, but don’t overthink every single reading – focus on the bigger patterns and trends.
The goal isn’t perfection; it’s progress. Each meal is an opportunity to make a choice that supports your health, and now you have the knowledge to make those choices count. Your future self will thank you, even if your present self thinks you’re crazy for eating pancakes at 7 AM.

