Gastric Sleeve Meal Plan Secrets That Actually Work (And Why Most Fail)

If you’ve had gastric sleeve surgery, you know that tiny stomach can feel like a blessing and a curse. One day you’re celebrating fitting into old jeans, the next you’re panicking because you can barely finish a few bites of scrambled eggs. I get it—and more importantly, I’ve helped hundreds of people figure out what actually works.
Your stomach size gets reduced by approximately 80% after gastric sleeve surgery, which means every single bite becomes incredibly important for your health and weight management goals. I’ve spent years researching what really works beyond basic portion control, and I’m going to share the simple brain science, gut health basics, and real-world social strategies that can transform your post-surgery relationship with food.
Here’s the thing nobody tells you: most people fail because they treat gastric sleeve meal planning like simple calorie counting. The real transformation happens at levels most patients never consider—from the good bugs in your gut to rewiring your brain’s response to food every time you eat.
Table of Contents
- The Truth About Your Gut Health After Surgery
- Those Critical First 72 Hours That Change Everything
- Why Hunger Comes Back (And How to Deal With It)
- Finding Your Personal Food Formula
- Surviving Social Situations Without Going Crazy
- How Quality Supplements Support Your Journey
TL;DR
- Your gut bacteria go through massive changes after surgery, and you need a simple plan to rebuild a healthy digestive system
- The first 72 hours create a critical window for gut reset that impacts how you’ll feel for months
- Hunger can return 6-12 months post-surgery when hormone production shifts, but strategic meal timing helps
- Your body type (how you process fats vs. carbs) determines your optimal food ratios for energy and satisfaction
- Eating in sequence (liquids, proteins, vegetables, then carbs) maximizes your limited digestive capacity
- Social eating requires new strategies since you can only manage 2-3 ounces per meal
- Simple environmental changes and consistent routines help rewire your brain’s relationship with food
The Truth About Your Gut Health After Surgery
Look, I know “gut bacteria” sounds like something only health nerds care about, but here’s the deal: after your sleeve surgery, your stomach isn’t just smaller—it’s like moving from a mansion to a studio apartment. Everything inside has to reorganize, including the tiny organisms that help you digest food.
I’ve watched too many people obsess over counting every calorie while completely ignoring what’s happening in their gut. Trust me, this stuff matters more than you think. When your stomach shrinks by 80%, those little bacteria go through major changes that directly affect whether you feel energized or exhausted, whether you absorb nutrients properly, and even how hungry you feel.
Research shows that for the first two months following gastric sleeve surgery, your calorie intake should be between 300 and 600 calories a day, with a focus on thin and thicker liquids, according to UCSF Health. That’s less than most people eat for breakfast, which is why every single bite has to work overtime to keep your body running.
Understanding the connection between digestive health and overall wellness becomes even more critical after gastric sleeve surgery. For those struggling with digestive discomfort during their recovery, learning about simple ways to beat bloat and improve digestion can provide immediate relief while your system adapts to its new capacity.
Here’s what I wish someone had told me: your digestive system after surgery is like starting a garden from scratch. You can’t just throw seeds everywhere and hope for the best. You need a plan.
Those Critical First 72 Hours That Change Everything
The first three days after your surgery aren’t just about healing—they’re like hitting the reset button on your entire digestive system. I know you’re probably focused on managing pain and sipping tiny amounts of water, but what’s happening inside is actually setting you up for how you’ll feel months from now.
Think of it this way: imagine your gut bacteria as tenants in an apartment building. Surgery is like a major renovation that forces most of them to move out. The first few days determine which new “tenants” move in to replace them. Get this part right, and you’ll have helpful neighbors. Mess it up, and you might deal with troublemakers for months.
Recent medical insights emphasize the importance of proper post-surgical nutrition planning. As “Norton Healthcare” reports, “The most successful patients have a combination of tools. They follow the nutrition plan, they pay attention to their bodies’ hunger and satiety [fullness] cues and they have the right mindset. If you haven’t done the mental work, it’s going to be much harder for you.”
One thing that really drives me crazy is when people think this is just about the surgery healing. Yes, that’s important, but you’re literally building the foundation for how your body will process food for the rest of your life during these first few days.
Your Step-by-Step Gut Recovery Plan
Okay, so here’s where most people get overwhelmed with complicated protocols. I’m going to break this down into simple steps that actually make sense.
Day 4: Start with something called acacia gum—sounds fancy, but it’s just a gentle fiber powder. Mix a tiny amount (like, quarter teaspoon tiny) into 2 ounces of water. This feeds the good bacteria without overwhelming your healing system. Think of it as offering a peace treaty to your gut.
Day 7: Here’s a weird trick that works: take a sweet potato, bake it, then stick it in the fridge overnight. The cooling process creates something called resistant starch (don’t worry about the science—just know it’s gut candy for good bacteria). Start with just one tablespoon of the mashed, cooled sweet potato.
Week 3: If you’re feeling adventurous and everything’s going well, you can try Jerusalem artichoke powder. Start with an eighth of a teaspoon—seriously, that’s barely anything, but it’s powerful stuff for building up your gut community.
The timing and type of nutrients you introduce during recovery can significantly impact your digestive comfort. Many post-surgery patients find that incorporating drinking vinegars for gut health during the later stages of recovery helps maintain the delicate bacterial balance established during the initial healing phase.
| Timeline | What to Add | How Much | Why It Helps |
|---|---|---|---|
| Day 4-6 | Acacia Gum | 1/4 tsp in 2 oz water | Gentle fiber for healing gut |
| Day 7-10 | Cooled Sweet Potato | 1 tbsp mashed | Feeds good bacteria |
| Week 2 | Green Banana | 1/4 small banana | Adds variety to gut food |
| Week 3 | Jerusalem Artichoke Powder | 1/8 tsp | Builds stronger gut community |
| Week 4+ | Mixed Gut-Friendly Foods | Small portions | Keeps everything stable |
I had a client, Maria, who skipped all this because it seemed “too complicated.” Three months later, she was dealing with constant bloating and fatigue. Once we went back and did this gut reset properly, she felt like a different person within two weeks.
The timing here isn’t arbitrary—it’s based on how your body actually heals and adapts. Rush it, and you’ll pay for it later. Take it slow, and you’re building a foundation that’ll serve you for years.
Understanding Your New Gut Neighborhood
Here’s something most doctors don’t explain: your stomach used to produce a lot of acid, and certain good bacteria loved that acidic environment. Now that you have way less stomach acid, those bacteria struggle to survive. It’s like the neighborhood changed, and some of your old friends can’t afford to live there anymore.
But here’s the good news: other beneficial bacteria actually prefer the new, less acidic environment. You just need to invite the right ones to move in.
Water kefir becomes your new best friend here—and before you ask, no, it doesn’t taste weird. Avoid the milk-based versions for now since your body might struggle with dairy initially. Think of water kefir as a gentle way to introduce the new beneficial bacteria that’ll thrive in your changed digestive system.
Sauerkraut juice is another powerhouse, but I’m not talking about the stuff in a jar from the grocery store. Look for properly fermented versions (they’ll be in the refrigerated section). Just one tablespoon daily provides specific bacterial strains that excel in lower-acid environments.
Sarah, one of my clients who’s a teacher, was struggling with energy crashes every afternoon about three months after surgery. We started her on one tablespoon of sauerkraut juice daily, gradually working up to two tablespoons, plus water kefir every other day. Within two weeks, her energy was steady all day, and her digestive issues completely disappeared.
The key is consistency, not perfection. You’re essentially training your gut to support your new lifestyle.
Why Hunger Comes Back (And What to Do About It)
Here’s what nobody warns you about: that amazing “I’m never hungry” feeling after surgery? It doesn’t last forever. Most people think hunger disappears permanently after gastric sleeve surgery, but around 6-12 months post-surgery, many patients notice their appetite creeping back.
Don’t panic—this is normal. What happens is your body gets creative. The hormone that makes you hungry (ghrelin) used to be produced mainly in your stomach. After surgery, your intestines start picking up the slack. It’s like your body finds a workaround.
But here’s the thing: you can actually use this to your advantage if you know what you’re doing.
Working With Your Body’s Natural Rhythm
Your hormones follow a daily schedule, whether you realize it or not. In the morning, your cortisol is naturally high (that’s what helps you wake up), and your body is primed to handle food efficiently. This is when you want to eat your biggest meal—which, let’s be honest, is still only about 3-4 ounces.
Medical guidelines recommend that daily caloric intake should not exceed 1,000 calories for gastric sleeve patients, according to UCSF Health. This makes meal timing crucial for maximizing the nutritional value and metabolic impact of every calorie consumed.
I recommend eating your main meal within two hours of waking up. I know this might seem backwards if you’re used to saving your “big” meal for dinner, but trust me on this. Your body can actually use those nutrients when your metabolism is firing on all cylinders.
Understanding your body’s natural rhythms becomes crucial for post-surgery success. The principles behind intermittent fasting for women can provide valuable insights into meal timing strategies that work synergistically with your reduced stomach capacity.
Plus, eating your main meal early helps prevent those afternoon cravings that can derail your progress. You know the ones—when you’re tired and everything sounds good, but you can only eat a few bites anyway, so you end up grazing all evening.
Training Your Brain to Feel Satisfied
This might sound weird, but every meal is actually a training session for your brain. You’re teaching it to recognize satisfaction from much smaller amounts of food. The key is slowing way down and really paying attention to what you’re eating.
Chew each bite 25-30 times. I know that sounds excessive, but you’re literally rewiring the connection between your brain and your stomach. Focus on the texture, the flavor, how it feels in your mouth. This isn’t just about digestion—you’re creating new neural pathways that help your brain feel satisfied with less food.
The Flavor Hack That Actually Works
Your brain’s reward system needs to adapt to finding satisfaction in tiny portions. This is where umami-rich foods become your secret weapon. Umami is that savory, satisfying taste that makes you feel like you’ve eaten something substantial.
Mushroom powder, nutritional yeast, and seaweed flakes might sound like health-food-store nonsense, but they’re actually powerful tools for making small portions feel more satisfying. A little sprinkle of nutritional yeast on your eggs or some mushroom powder in your soup can make your brain feel more rewarded, even though you’re eating the same small amount.

Finding Your Personal Food Formula
Here’s where most meal plans get it completely wrong: they assume everyone’s body works the same way. But the truth is, some people thrive on higher fat, others need more carbs, and some need protein at every meal to feel steady. After surgery, when you can only eat tiny amounts, getting this right becomes even more critical.
I’ve seen people follow identical meal plans with completely different results. The successful ones figured out their personal formula—the others struggled with constant fatigue, cravings, or just feeling “off” all the time.
Reading Your Body’s Signals
Your body gives you clues about what it needs, but you have to know how to read them. This goes way beyond basic hunger and fullness—I’m talking about energy patterns, mood changes, how well you sleep, even things like hair and nail health.
Research indicates that gastric sleeve patients should aim for a minimum of 65 to 75 grams of protein a day, though many can’t reach this goal in the first few months after surgery, according to UCSF Health. How efficiently you process this protein depends on your individual body type.
If you tend to have thick hair, strong nails, and feel more energetic in the evening, you probably process fats and proteins more efficiently than carbohydrates. Your ideal meal should be about 60% healthy fats (think avocado, nuts, olive oil), 30% protein, and only 10% complex carbs.
On the flip side, if you have fine hair, tend to feel anxious, and crash in the afternoon, your system burns through nutrients quickly. You’ll probably feel better with 50% complex carbohydrates, 30% protein, and 20% fats, eating every 2-3 hours to keep your blood sugar steady.
I had a client named Mark who initially tried following a high-fat meal plan because that’s what his support group was doing. He felt terrible—constantly tired and irritable. Once we switched him to higher-carb meals with sweet potato, quinoa, and more frequent eating every 2.5 hours, his energy stabilized and he lost an additional 15 pounds over three months.
The point is, there’s no one-size-fits-all approach. You have to experiment and pay attention to how your body responds.
Making Every Bite Count
When you can only eat 2-3 ounces per meal, every single bite needs to be strategic. Your stomach is producing way less digestive acid and enzymes than it used to, so you need to be smart about food combinations and timing.
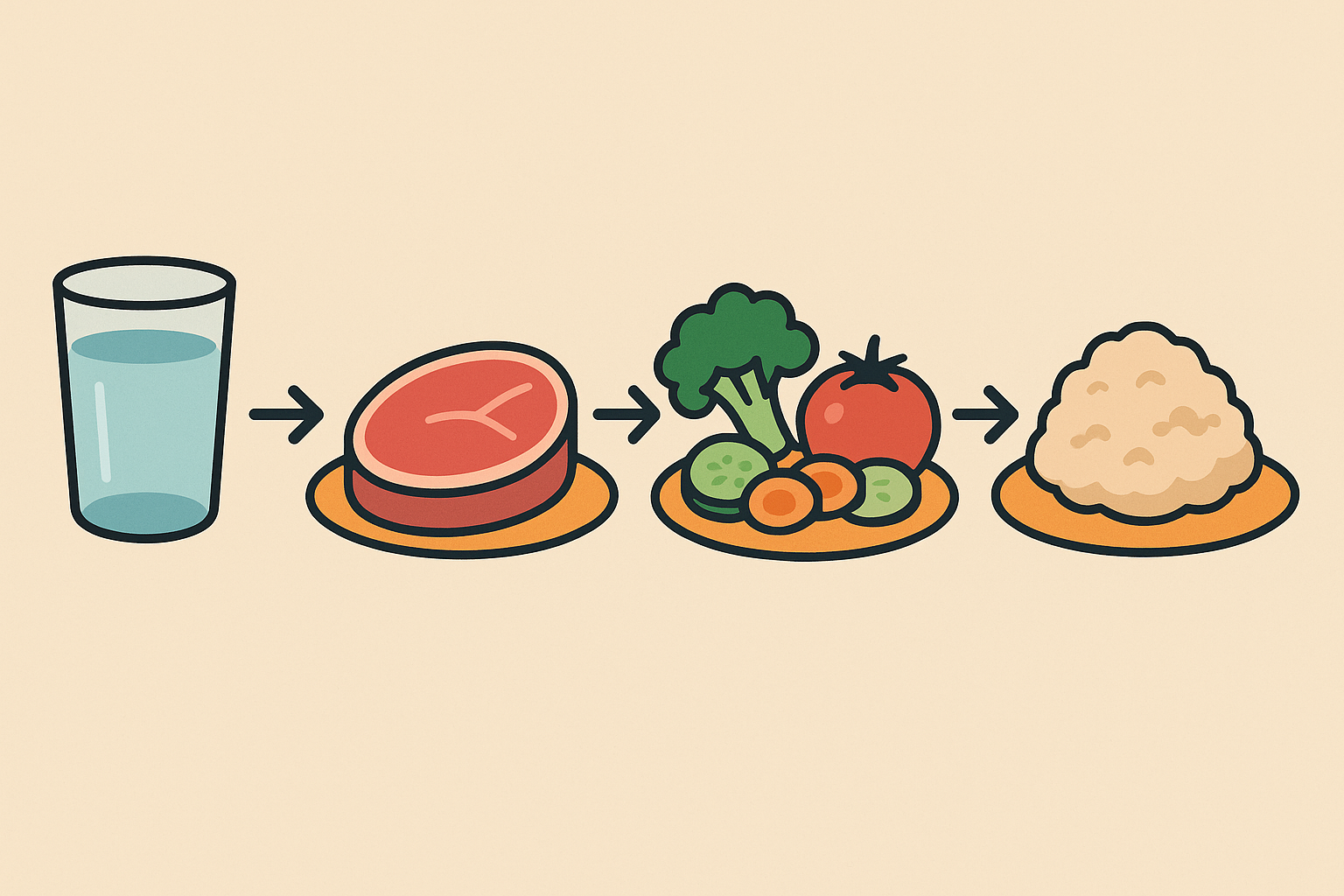
The Order That Actually Matters
This might sound obsessive, but the order you eat foods in can make a real difference in how you feel and how well you absorb nutrients. Here’s what I recommend:
First: Liquids (bone broth, herbal tea, or just water)
Second: Proteins (these need the most stomach acid to break down)
Third: Vegetables
Last: Any complex carbohydrates
This sequence maximizes your limited digestive capacity and helps prevent that uncomfortable “too full” feeling that can hit suddenly.
Nutrient Timing That Makes Sense
Some nutrients actually compete with each other for absorption, which becomes a bigger deal when you can only eat small amounts. For example, iron and calcium block each other, so don’t eat iron-rich foods (like beef) at the same time as calcium-rich foods (like leafy greens). Space them at least two hours apart.
But vitamin C actually helps iron absorption, so pairing beef with bell peppers or spinach with strawberries is smart. These aren’t random rules—they’re based on how your body actually processes nutrients.
| Nutrient Combination | Timing | Effect | Example Foods |
|---|---|---|---|
| Iron + Vitamin C | Same meal | Enhanced absorption | Beef + bell peppers |
| Iron + Calcium | 2 hours apart | Prevents competition | Beef, then leafy greens |
| Fat + Fat-soluble vitamins | Same meal | Improved uptake | Avocado + vitamin D supplement |
| Zinc + Protein | Same meal | Better absorption | Pumpkin seeds + chicken |
| B12 + Folate | Same meal | Synergistic effect | Nutritional yeast + spinach |
Getting Your Hormones Back on Track
Your smaller stomach affects way more than just digestion—it changes your entire hormone production. Understanding this can prevent a lot of common issues that catch people off guard months after surgery.
Why You Might Not Feel Satisfied
Leptin is the hormone that tells your brain “okay, I’m full now.” With less stomach tissue producing leptin, your brain might struggle to get that satisfied signal. This is why some people feel like they could keep eating even after their tiny stomach is physically full.
Including zinc-rich foods and omega-3 fatty acids from sources like wild-caught sardines helps restore leptin sensitivity. It’s not an instant fix, but over time, it helps you feel truly satisfied with your smaller portions instead of constantly fighting the urge to eat more.

Surviving Social Situations Without Going Crazy
Let’s talk about the elephant in the room: eating out, family dinners, work events, and all those social situations that revolve around food. When you can only eat a few bites, these situations can feel awkward, isolating, or just plain stressful.
The growing awareness of alternative weight loss approaches is highlighted by recent success stories. A 50-year-old woman from London recently made headlines by “rejecting gastric sleeve surgery” and instead choosing a structured meal replacement program, demonstrating that psychological commitment to portion control can be successful regardless of the chosen method.
I’ve had clients who started avoiding social events altogether because they felt embarrassed about their eating habits. That’s not living—that’s hiding. Here are some strategies that actually work in real life.
Rewriting the Rules of Social Eating
The key is shifting your focus from eating to connecting. I know that sounds easier said than done, but hear me out.
Before you go: Eat your planned meal at home. This takes the pressure off and ensures you get proper nutrition instead of trying to make a restaurant meal work with your needs.
At the event: Order something small to share or just a side dish. Position yourself as the conversation facilitator—ask people about their lives, their work, their kids. Most people love talking about themselves and won’t even notice you’re not eating much.
Have a standard response ready: When people comment on your eating (and they will), have a simple response like “I had a late lunch” or “I’m not very hungry right now.” You don’t owe anyone an explanation about your surgery or eating habits.
The psychological aspect of changing your relationship with food extends beyond just meal planning. Learning about intuitive eating principles can help you develop a healthier mindset around food choices, even when working within the constraints of your reduced stomach capacity.

Redesigning Your Home Environment
Your brain needs new visual cues to support your new eating patterns. This isn’t about willpower—it’s about making the healthy choice the easy choice.
Use smaller plates—6-inch diameter maximum. Eat with dessert spoons instead of regular utensils. Create a specific eating space that’s separate from where you used to eat larger meals. These small changes help your brain adjust to smaller portions without feeling deprived.
One of my clients, Jennifer, bought a set of beautiful 6-inch ceramic plates and cocktail forks. She set up a small corner table as her “mindful eating space” with a special placemat and cloth napkin. This environmental redesign helped her brain associate smaller portions with a special, intentional experience rather than feeling restricted.
Dealing with Your Changing Identity
Here’s something nobody talks about: if you used to be “the foodie” in your friend group, or if cooking and entertaining was a big part of your identity, surgery can feel like you’re losing part of who you are.
The good news is you can channel that food passion in new directions. Become the expert on nutrient density, high-quality ingredients, or cooking techniques for small portions. You can still be the person friends turn to for food advice—you’re just approaching it from a different angle.
Instead of being known for eating large amounts or cooking huge meals, you can become known for quality over quantity. You might discover amazing local farmers’ markets, learn about sourcing the best ingredients, or master techniques for making small portions incredibly flavorful and satisfying.
How Quality Supplements Support Your Gastric Sleeve Journey
Let’s be realistic: even with perfect meal planning, getting all your nutrients from 600-800 calories a day is challenging. This is where high-quality supplements become essential, not optional.
Navigating the complex nutritional demands of post-gastric sleeve life becomes significantly easier with the right support and high-quality supplements. Organic Authority’s commitment to clean, bioavailable ingredients aligns perfectly with the elevated focus on nutrient density that your reduced stomach capacity demands. When you can only consume 2-3 ounces per meal, every ingredient must be purposefully chosen and optimally absorbed.
But here’s the thing—not all supplements are created equal. When your digestive capacity is limited, you need supplements that are easily absorbed and gentle on your system. You can’t afford to waste money on cheap vitamins that your body can’t use.
Marine collagen, for example, provides easily absorbed protein that’s gentle on your sensitive digestive system while supporting skin, hair, and nail health during rapid weight loss. B12, iron, vitamin D, and calcium become critical because gastric sleeve patients are at higher risk for these deficiencies.
The brand’s rigorous evaluation and approval processes mirror the careful, scientific approach needed for successful gastric sleeve meal planning. Their targeted supplements address the specific deficiency risks that gastric sleeve patients face—from B12 and iron to vitamin D and calcium.
What I appreciate most is how Organic Authority builds community around wellness routines, which directly addresses the social psychology challenges we’ve discussed. Having a supportive environment for navigating your transformed relationship with food makes all the difference in long-term success.
Ready to optimize your post-surgery nutrition with clean, effective supplements? Explore Organic Authority’s carefully vetted products designed to support your wellness journey.

The Real Talk About Long-Term Success
Your gastric sleeve journey doesn’t end when you hit your goal weight. In many ways, that’s when the real work begins—maintaining your new lifestyle and relationship with food for the long haul.
Success isn’t just about the number on the scale. It’s about building a sustainable way of eating that honors your body’s new capacity while meeting your nutritional needs. It’s about navigating social situations with confidence. It’s about feeling energetic and healthy, not just smaller.
The strategies we’ve covered—from gut health to finding your personal food formula to social navigation—work together to create a comprehensive approach that supports both your physical and emotional well-being. But remember, this is a marathon, not a sprint.
Be patient with yourself as you implement these changes. Your brain needs time to form new habits, your gut bacteria need weeks to establish healthy colonies, and your social identity will evolve gradually. Every small step you take toward understanding and working with your body’s new reality brings you closer to the healthy, vibrant life you’re working toward.
Most importantly, remember that you’re not alone in this journey. The challenges you’re facing—from figuring out what to eat to navigating social situations—are things thousands of people have successfully worked through. You can do this too.

