Post Bariatric Surgery Meal Plan: What I Wish Someone Had Told Me About the Hidden Challenges

Table of Contents
- The Vitamin Nightmare That Almost Broke Me
- Why Everything You Think You Know About Protein Is Wrong
- The Weird Gut Changes Nobody Warns You About
- Throwing Out the Meal Schedule Rulebook
- How I Became My Own Food Detective
- Surviving Dinner Parties Without Losing Your Mind
- Making This Work When Life Gets Messy
- Why Clean Food Became My Non-Negotiable
TL;DR
- Your body not getting the vitamins it needs can sabotage everything, even when you’re following your meal plan perfectly
- When you eat matters more than most doctors tell you – there are specific windows when your body can actually absorb stuff
- Your gut bacteria goes completely haywire after surgery, messing with everything from your mood to what you crave
- Being flexible with when you eat beats following rigid schedules every time
- Glucose monitors and other gadgets can show you exactly how your body reacts to different foods
- Family drama and social eating need their own game plan
- Long-term success means changing your approach as your life changes
- Quality supplements and clean foods become essential when your body can barely absorb anything
The Vitamin Nightmare That Almost Broke Me
I remember standing in my kitchen at 2 AM, six months after surgery, crying over a bowl of scrambled eggs I couldn’t finish. I was doing everything my doctor told me to do, but I felt like garbage. My hair was coming out in clumps, I could barely drag myself through the day, and I was starting to panic that I’d made a terrible mistake.
Here’s the thing nobody tells you: you can follow your post bariatric surgery meal plan to the letter and still feel awful if you’re not getting the vitamins your body needs. I hit my protein targets, measured my portions religiously, and took my prescribed multivitamin. But I was completely missing how my altered digestive system actually processes vitamins and minerals.
The post bariatric surgery meal plan progresses through 4 carefully structured stages over the first 4 to 6 weeks, with each phase designed to gradually reintroduce different food textures as your body heals. During this critical period, patients must work up to at least 7½ cups (60 ounces) of fluid daily to prevent dehydration – which becomes even trickier when you’re trying to time everything perfectly.

Learning When Your Body Can Actually Absorb Stuff
Your surgery didn’t just make your stomach smaller – it completely changed when and where your body can absorb different nutrients. I learned the hard way that there are specific time windows when absorption works best, and missing these windows means you’re basically flushing money and nutrients down the drain.
Understanding which supplements are essential for daily intake becomes crucial when your body’s ability to absorb nutrients is compromised after surgery. I had to become a detective, figuring out which nutrients fought with each other and which ones actually helped each other work better.
| Nutrient | Best Time to Take | What Helps It Work | What Screws It Up |
|---|---|---|---|
| Iron | Morning, empty stomach | Vitamin C, meat | Calcium, coffee, tea |
| Calcium | Split up, with meals | Magnesium, Vitamin D | Iron, high-fiber foods |
| B12 | Under the tongue, between meals | Folate | Alcohol, antacids |
| Fat vitamins (A,D,E,K) | With healthy fats | MCT oil, avocado | Mineral oil |
| Zinc | Empty stomach or bedtime | Copper | Iron, calcium |
Figuring Out Your Personal Vitamin Highway
Different surgeries mess with nutrient absorption in different ways. If you had gastric bypass like me, certain nutrients literally can’t be absorbed in the same places anymore. I had to learn which nutrients needed to be kept apart, which ones worked better together, and exactly when my body was ready to actually use what I was giving it.
The gastric bypass diet requires extra careful attention to when you take things since the procedure bypasses a big chunk of your small intestine where absorption usually happens. My surgeon explained the anatomy changes, but nobody prepared me for what that actually meant day-to-day.
Here’s a perfect example: I spent three weeks religiously taking my iron supplement with my morning coffee, wondering why I still felt exhausted. Turns out coffee blocks iron absorption. Whoops. Sometimes the learning curve feels more like a learning cliff. I switched to taking iron with vitamin C-rich foods like strawberries on an empty stomach, then waiting two hours before my coffee. My iron levels improved dramatically within three months.
Turning Dumping Syndrome Into Your Body’s Feedback System
Instead of just trying to avoid dumping syndrome, I learned to use it as valuable information about what my body could and couldn’t handle. The sweating, nausea, and racing heart weren’t just punishments – they were my body’s way of telling me exactly which food combinations overwhelmed my new digestive system.
I started keeping a detailed log of every episode, noting what I ate, when I ate it, and how bad the symptoms were. After a few months, I could predict exactly which combinations would send me running to the bathroom and which ones my body could handle just fine.

The Protein Game-Changer Nobody Talks About
Here’s the cruel irony: you need way more protein while having way less ability to digest it. I had to completely rethink how I approached protein, moving way beyond just “eat more chicken” to understanding how to set up my digestive system for success and actually use every gram I managed to get down.
According to “Norton Healthcare’s post-surgery nutrition guidelines”, patients progress from liquid protein shakes in the first two weeks to introducing soft proteins like scrambled eggs and finely chopped meats at the two-week mark, emphasizing that protein should be prioritized at each meal throughout the recovery process.
The gastric bypass diet makes protein tricky because your stomach acid production drops significantly after surgery. Without enough stomach acid, protein digestion becomes a mess, leading to deficiencies even when you’re eating plenty.
Setting Your System Up for Protein Success
I discovered that taking specific digestive enzymes before meals and incorporating fermented proteins dramatically improved how much protein my body actually used. The importance of improving digestion naturally becomes even more critical when your stomach is the size of an egg and every nutrient has to count.
Creating the right conditions for protein digestion required completely overhauling my eating routine. I had to think about enzyme production, stomach acid levels, and chewing – all while working with a tiny stomach.
My Pre-Meal Protein Setup:
- Take digestive enzymes 15 minutes before eating
- Make sure I have enough stomach acid with lemon water or apple cider vinegar
- Choose easily digestible proteins (fish, eggs, protein powder)
- Eat protein first, before anything else
- Chew thoroughly and eat slowly (minimum 20 minutes per meal)
- Don’t drink anything 30 minutes before or after meals
The Weird Gut Changes Nobody Warns You About
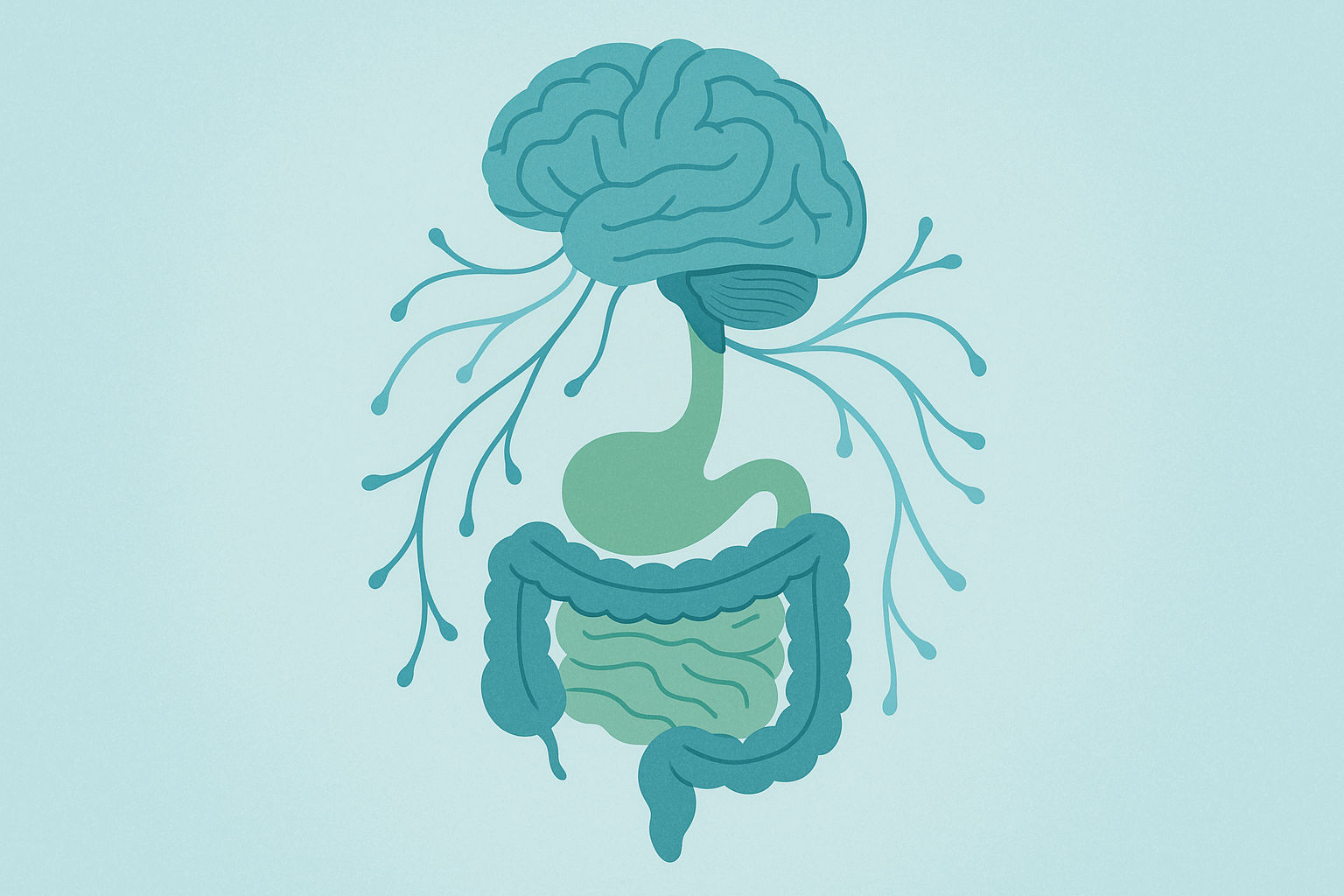
The changes in your gut bacteria after surgery affect way more than just digestion – they mess with your mood, cravings, and even how your brain responds to food. I had to learn how to actively rebuild my gut health and use specific nutrients to literally rewire how my brain thought about food.
Three months post-surgery, I noticed my food cravings had completely flipped. Foods I used to love suddenly seemed gross, while others I’d never enjoyed became intensely satisfying. Turns out bariatric surgery dramatically changes your gut bacteria, which talks directly to your brain through the vagus nerve.
Feeding the Good Bacteria (And Starving the Bad Ones)
I learned to design meals that specifically fed the good bacteria while creating an environment where the troublemaker bacteria couldn’t survive. This meant incorporating specific amounts of prebiotics, rotating fermented foods strategically, and using targeted antimicrobial foods during reset phases.
Supporting gut health through drinking vinegars and fermented foods can help rebuild the microbiome that gets disrupted by surgery and medication. I had to be careful about introducing these foods gradually since my sensitive post-surgical digestive system couldn’t handle large amounts at first.
My daily gut-support routine included starting each morning with a small serving of sauerkraut (packed with good bacteria), followed by a prebiotic-rich snack like a small apple with almond butter later in the day. I rotated between different fermented foods weekly – kimchi, kefir, and miso – to introduce variety while not overwhelming my sensitive system.
Using Food to Rewire Your Food Brain
Certain nutrients can actually help rebuild the brain pathways that control food cravings and feeling full. I started timing omega-3s, magnesium, and B-vitamins strategically to support brain chemical production and used adaptogenic herbs to break the stress-eating cycle that had controlled me for years.
The connection between not getting enough nutrients and feeling terrible became crystal clear when I started tracking both at the same time. Low B12 levels matched up perfectly with my worst anxiety days, while not getting enough omega-3s preceded periods of intense food cravings and emotional eating episodes.
Throwing Out the Meal Schedule Rulebook
The standard “eat small frequent meals” advice only scratches the surface of what’s actually possible. I discovered that building flexibility – the ability to efficiently switch between different fuel sources – was way more powerful than following rigid meal timing rules. This approach helped me maintain stable energy and mood while supporting my body’s healing process.
The gastric bypass diet doesn’t have to mean being chained to a clock. After months of forcing myself to eat every two hours regardless of whether I was hungry or full, I realized I was working against my body’s natural rhythms instead of with them.
Strategic Keto Phases for Post-Surgery Bodies
Using ketogenic phases strategically sped up my fat loss, reduced inflammation, and improved my insulin sensitivity. But doing keto after bariatric surgery isn’t the same as regular keto – different procedures require different approaches based on how they affect fat absorption and metabolism.
Learning how to determine your personal carb tolerance is essential for safely doing strategic ketosis phases after bariatric surgery. I had to account for my reduced bile acid production and altered fat absorption when calculating my ratios.
Customizing Keto for Your Specific Surgery
I had to figure out personalized ketone targets based on my surgery type and current healing phase. This meant monitoring ketone production through testing and adjusting my fat sources based on my body’s actual bile acid production, rather than following generic keto guidelines.
| Surgery Type | Fat Absorption | Recommended MCT Oil | Ketone Target | How Often to Check |
|---|---|---|---|---|
| Gastric Sleeve | 85-90% of normal | 1-2 tbsp daily | 0.5-1.5 mmol/L | 2x weekly |
| Gastric Bypass | 60-70% of normal | 2-3 tbsp daily | 0.8-2.0 mmol/L | Daily at first |
| Duodenal Switch | 40-50% of normal | 3-4 tbsp daily | 1.0-2.5 mmol/L | Daily |
| Gastric Band | 95% of normal | 1 tbsp daily | 0.5-1.0 mmol/L | Weekly |
Making Intermittent Fasting Work With Your New Body
Modified intermittent fasting can work beautifully with your smaller stomach, but you have to adapt the approach rather than forcing your post-surgical body into standard fasting windows. I learned to work with my body’s new rhythms instead of against them.
Understanding how women should approach intermittent fasting provides valuable insights for post-bariatric patients who need to modify traditional fasting approaches. Hormone considerations become even more important when your body is already adapting to major changes.
Syncing Your Eating Windows With Your Body Clock
I discovered that aligning my eating patterns with my natural hormone fluctuations helped me actually use nutrients better and supported the healthy sleep patterns that were crucial for my recovery. This meant figuring out my personal chronotype and using light therapy to support my circadian rhythm.
My cortisol patterns had shifted dramatically after surgery, peaking earlier in the morning and dropping more sharply in the evening. By timing my largest meal during my natural cortisol peak, I improved both digestion and energy levels throughout the day.
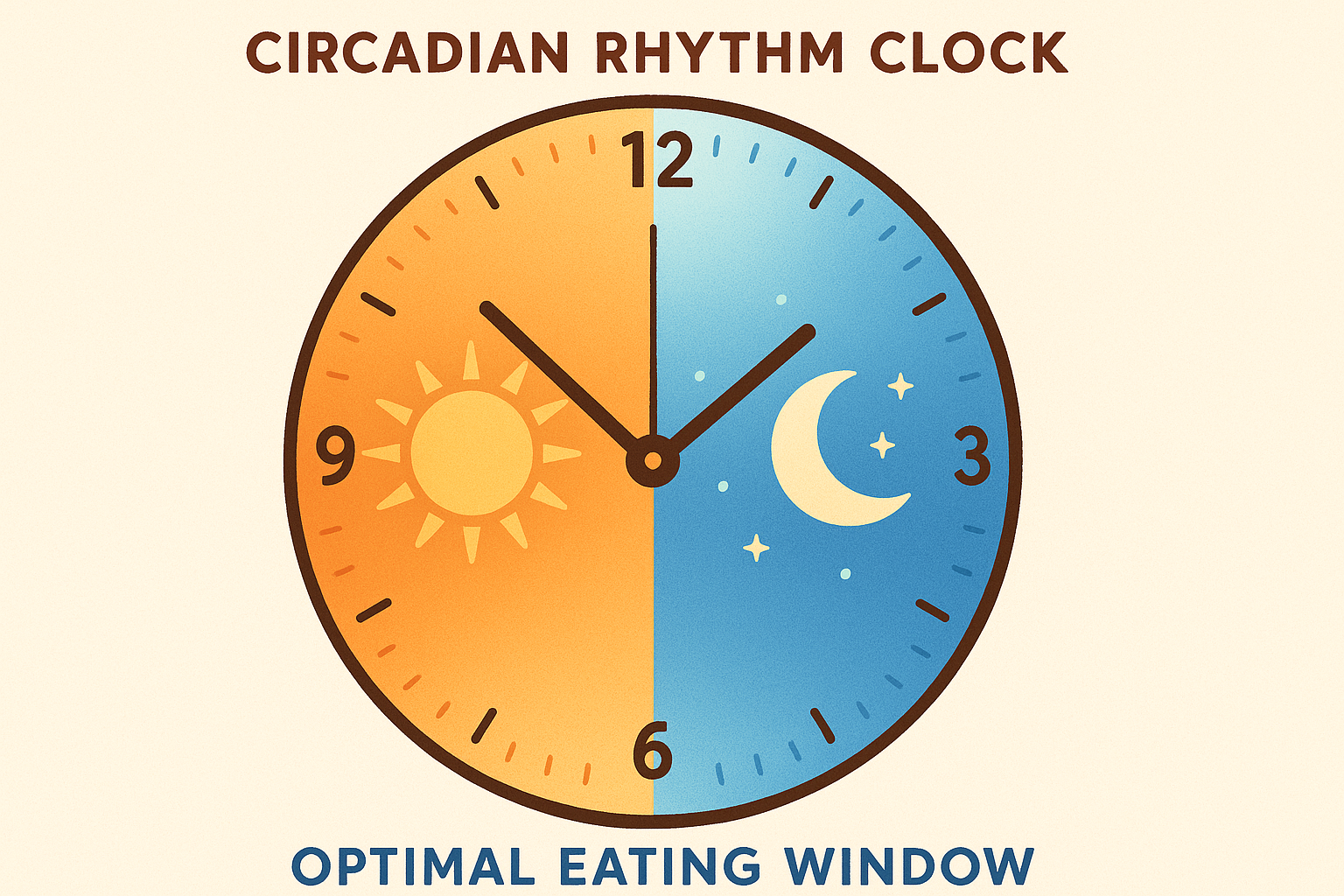
Triggering Your Body’s Cellular Cleanup Mode
Strategic fasting periods can activate autophagy – your body’s cellular cleanup process – which supports long-term health outcomes beyond just weight loss. I learned to gradually extend fasting windows while monitoring my energy levels and timing my fast-breaking meals with the most nutrient-dense, easily digestible foods.
The key was starting with shorter fasting windows and gradually extending them based on how my body responded. I began with 12-hour overnight fasts and slowly worked up to 16-hour windows, always prioritizing nutrient density when breaking my fasts.
How I Became My Own Food Detective
Generic meal plans can only take you so far. I learned to use wearable technology and regular lab work to create meal plans that actually responded to my changing needs and healing progress in real-time, rather than following static guidelines that might not work for my unique situation. This data-driven approach completely changed how I approached my gastric bypass diet.
I’m not a tech person, but the turning point came when I realized I was making food decisions based on guesses rather than actual data about how my body was responding to different foods and timing strategies.
Becoming Your Own Body’s Translator
Continuous monitoring of my body’s signals transformed how I approached meal planning. Instead of guessing what worked, I could see exactly how different foods affected my body and adjust accordingly. This eliminated so much trial and error and helped me optimize my results way faster.
I started tracking everything: blood sugar responses, ketone levels, sleep quality, energy ratings, and mood scores. The patterns that emerged were fascinating and completely personalized to my unique body and surgical changes.
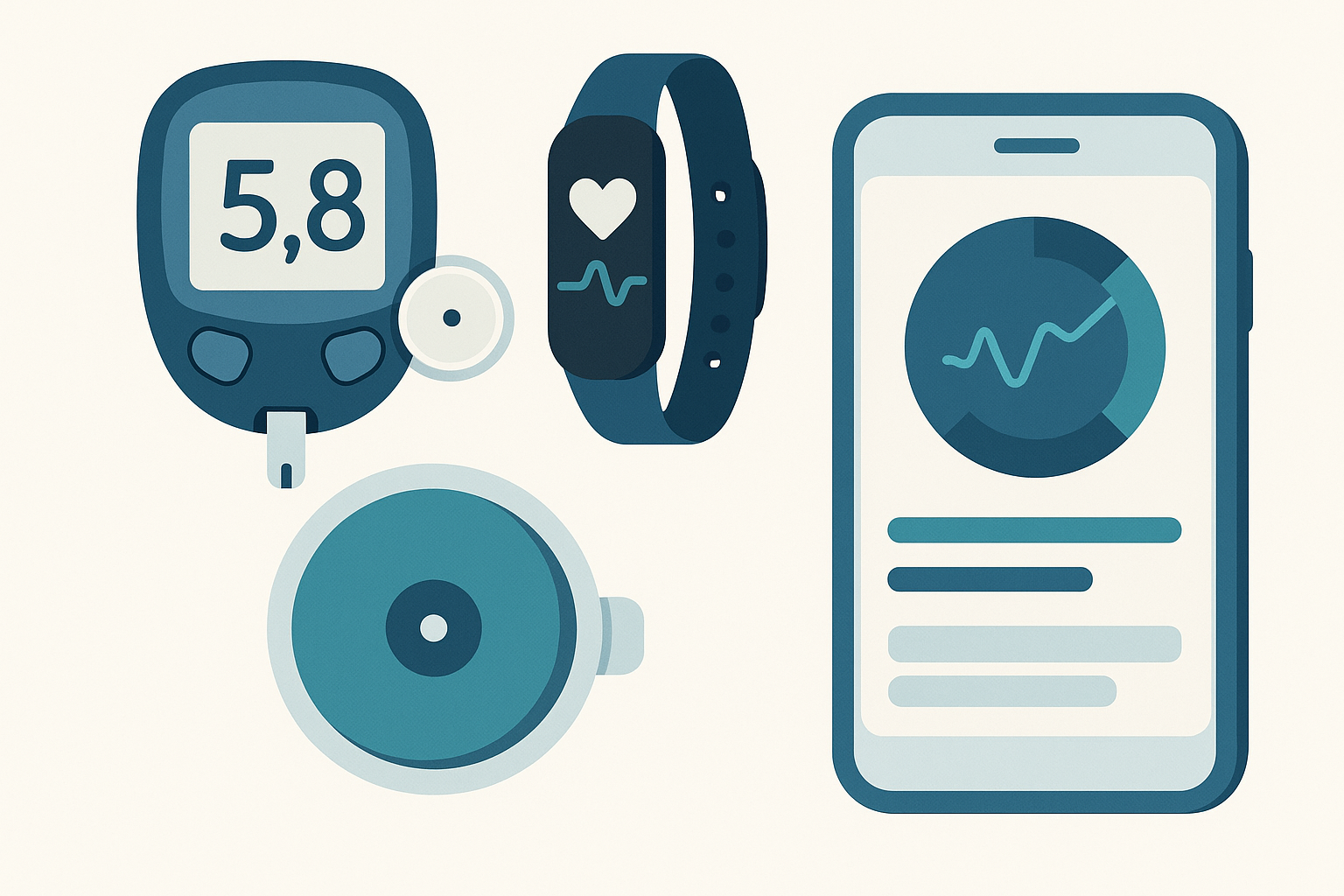
Reading Your Blood Sugar Like a Book
Using a continuous glucose monitor was like having a conversation with my body for the first time. It told me that sweet potatoes made my blood sugar go crazy, but butternut squash was totally fine. Who would have guessed? This data helped me create my personalized “green light” foods list – butternut squash became a staple, while sweet potatoes moved to my “special occasion only” category.
The glucose data also revealed that my body processed carbs completely differently at different times of day. Morning carbs caused minimal spikes, while the same foods in the evening sent my glucose soaring and messed up my sleep.
I started simple – just wrote down what I ate and how I felt afterward in a little notebook. Turns out I felt like garbage every time I ate anything with sugar alcohols. Who needs fancy apps when a $2 notebook can save you from hours of stomach pain?
Surviving Dinner Parties Without Losing Your Mind
The social and psychological parts of post-bariatric eating are rarely talked about in meal plans, but they’re absolutely crucial for long-term success . I had to learn how to navigate family dynamics, workplace eating challenges, and social gatherings while managing my own evolving relationship with food – all without isolating myself or compromising my health.
The first time I went to a restaurant after surgery, I ordered a $28 salmon dish and could only manage three tiny bites. The server kept asking if something was wrong with the food, my dining companions looked concerned, and I wanted to crawl under the table. I ended up taking home a doggy bag that lasted me three meals.
Dealing With Family Food Drama
Becoming the catalyst for household nutrition changes while managing family resistance was one of my biggest challenges. My husband felt like he was walking on eggshells around me. He’d apologize for eating a sandwich in front of me, and I’d get defensive because I didn’t want to be treated like a fragile patient. We had some pretty ugly fights about food before we figured out how to talk about this stuff without both of us feeling terrible.
Research from “Hartford HealthCare’s bariatric nutrition team” emphasizes that patients should prioritize protein first, followed by vegetables, and limit carbohydrates to around 50 grams per day, with the recommendation that “the more food is processed, the less likely it is to be good for you.”
I learned that involving family members in my specialized meal preparation actually created stronger support systems while educating them about my new needs and limitations. My family initially struggled with my tiny portions and specific food requirements. They felt guilty eating normal-sized meals in front of me and worried constantly about saying the wrong thing about food. We had to establish new communication patterns and meal routines that worked for everyone.

Making Meal Prep a Team Effort
I started creating family meal prep sessions focused on recipes that worked for my portions and needs. We established “safe zones” in the kitchen for my post-surgical foods and developed ways to talk about food choices without anyone feeling bad.
Sunday Planning Session (30 minutes):
- Review upcoming week’s schedules and eating challenges
- Select 3-4 base proteins that work for everyone
- Plan vegetable sides that can be prepared multiple ways
- Identify potential problem meals and create alternatives
Prep Day Jobs:
- Protein prep: Batch cook chicken, fish, and eggs
- Vegetable prep: Wash, chop, and portion vegetables
- Sauce/seasoning station: Prepare family-friendly seasonings
- Storage: Portion individual servings in clearly labeled containers
Mastering Social Eating Without Becoming a Hermit
Restaurants, parties, and social gatherings required planning strategies that let me maintain my social connections while sticking to my nutritional requirements. I learned to research menus ahead of time, practice estimating portions using visual cues, and develop polite ways to deflect well-meaning but inappropriate food offers.
I developed responses for common social eating situations. When someone insisted I try their homemade dessert, I’d say, “It looks amazing! Could you wrap up a small piece for me to take home?” This satisfied their need to share while giving me control over if and when I consumed it.
Navigating Workplace Food Challenges
Professional environments presented unique obstacles – from limited refrigeration to meeting schedules that conflicted with my eating requirements. Let me tell you about the office birthday cake situation. There I was, three months post-surgery, and Karen from accounting is practically shoving chocolate cake in my face saying “just one bite won’t hurt!” I wanted to scream “Lady, one bite could send me to the bathroom for an hour!” Instead, I smiled and said I’d save it for later. Pro tip: always have an exit strategy.
Office birthday parties became minefields. Conference room meetings scheduled during my planned meal times created logistical nightmares. Business lunches required diplomatic navigation between professional relationships and my dietary restrictions.

Creating Your Office Nutrition Command Center
I learned to stock non-perishable protein sources and emergency snacks in my desk, establish relationships with nearby restaurants that could accommodate my needs, and create meeting schedule buffers that allowed for proper meal timing without affecting my professional responsibilities.
My desk drawer became a mini nutrition pharmacy: protein powder packets, nuts, jerky, and emergency supplements. I identified three nearby restaurants with grilled protein options and established relationships with the staff who understood my portion needs.
Managing Professional Boundaries Around Food
Deciding whether and how to tell colleagues about my surgical status while maintaining professional boundaries and ensuring my nutritional needs were met required careful strategy. I developed standard responses to food-related invitations that didn’t require disclosure and identified trusted colleagues who could provide support during challenging eating situations.
I chose to tell my immediate supervisor about my surgery for practical reasons – I needed flexibility for follow-up appointments and occasional energy fluctuations during my recovery. However, I kept the information private from most colleagues, developing neutral responses to food-related questions that didn’t invite further inquiry.
Making This Work When Life Gets Messy
Moving beyond the initial recovery phase required developing sustainable systems that could evolve with changing life circumstances, seasonal variations, and aging-related metabolic changes. I had to think beyond the first year and create frameworks that would adapt as my life changed.
Two years in, I thought I had it all figured out. Then I got a promotion, started working longer hours, and my whole eating schedule went to hell. I was grabbing protein bars for dinner and wondering why I felt awful. Sometimes you have to give yourself permission to start over, even when you think you should have it mastered by now.
Adapting to Your Body’s Seasonal Moods
I discovered that post-bariatric patients often experience heightened sensitivity to seasonal changes in food availability, mood, and energy levels. My first winter after surgery nearly broke me. The shorter days made me want to hibernate, and all I wanted was comfort food I couldn’t eat. I found myself standing in front of the pantry at 9 PM, staring at crackers I couldn’t have, feeling sorry for myself. That’s when I realized I needed a winter game plan.
Winter brought unique challenges: reduced sunlight affected my vitamin D levels, seasonal depression triggered old emotional eating patterns, and holiday food traditions required constant navigation. I learned to anticipate these patterns and adjust my supplementation and meal planning accordingly.
Planning for Life’s Curveballs
Major life events like career changes, relationships, or health issues require specialized adaptations to post-bariatric meal plans. I learned to create flexible systems that could rapidly adapt to changing circumstances and develop emergency protocols for periods when normal eating patterns might be disrupted.
When I changed jobs and my commute doubled, my entire meal timing structure collapsed. I had to redesign my nutrition strategy around longer days, different stress patterns, and limited food preparation time. Having flexible frameworks in place made this transition manageable rather than catastrophic.
Life Event Nutrition Backup Plan:
- Identify potential disruptions to meal timing and preparation
- Create portable nutrition backup plans (shelf-stable proteins, supplements)
- Establish support network contacts for meal assistance
- Develop stress-eating prevention strategies
- Plan for medication timing changes that affect nutrient absorption
- Create simplified meal templates for high-stress periods
Here’s something weird nobody prepared me for – my taste buds completely changed. Foods I used to love tasted like cardboard, and things I never cared about suddenly seemed amazing. I became obsessed with pickles. Like, seriously obsessed. Your body is going to surprise you in ways you can’t predict.
Why Clean Food Became My Non-Negotiable
With compromised absorption capacity, the quality of foods and supplements becomes absolutely critical. I used to think organic was just marketing hype for people with too much money. But when your body can barely absorb half of what you eat, you realize you can’t afford to waste it on junk. It’s like having a tiny gas tank – you better put premium fuel in there.
Post-bariatric surgery patients can’t afford to consume foods with hidden additives or contaminants that could disrupt their delicate digestive balance. When your body can only absorb a fraction of what you consume, every nutrient needs to count. That’s where Organic Authority’s commitment to clean, effective nutrition becomes invaluable.
Their marine collagen provides superior absorption for tissue repair and wound healing – critical during the post-surgical period. The plant-based digestive support supplements align perfectly with the need to rebuild and maintain a healthy microbiome after surgery. When you’re working with limited absorption capacity, you need supplements that meet the highest standards for purity and bioavailability.
Ready to optimize your post-bariatric nutrition with clean, effective products? Explore Organic Authority’s carefully curated selection of supplements designed to support your body’s incredible capacity for healing and transformation.
Final Thoughts
If I could go back and tell myself one thing on day one, it would be this: it gets easier, but it never gets automatic. You’ll always have to think about food differently than other people, and that’s okay. You’re not broken – you’re just playing by different rules now.
What surprised me most was how much the psychological and social aspects mattered. You can have the perfect meal plan on paper, but if you can’t navigate a family dinner or handle workplace eating situations, you’re setting yourself up for struggle.
The technology piece was a game-changer too. Being able to see exactly how my body responded to different foods eliminated so much guesswork and helped me fine-tune everything much faster than trial and error alone.
Most importantly, I learned that this isn’t a temporary phase you get through – it’s a complete lifestyle transformation that needs to evolve as you do. The systems and strategies that work in year one might need adjustments in year three, and that’s completely normal.
Some days you’ll nail it – hit your protein goals, take all your vitamins, feel like a champion. Other days you’ll eat three bites of chicken and call it dinner. Both days are part of the process. This isn’t about being perfect; it’s about showing up and trying again tomorrow.
Find your people – the ones who get it. Whether that’s an online support group or that one friend who asks how you’re really doing. This journey is too hard to do alone, and there’s no shame in needing help figuring it out.
Your post-bariatric surgery meal plan should be as unique as you are. Take what resonates from my experience, adapt it to your situation, and remember that the goal isn’t perfection – it’s progress and sustainability. Look, this stuff is hard. You’re basically learning to feed a completely different body while everyone around you eats normally. Give yourself some grace. You’re figuring it out as you go, just like the rest of us.

